Pandemic: COVID-19 (2020)

Photo by: Immo Wegmann (Unsplash)
Study offers a mental well-being 'tool kit' anyone can use
Researchers at the University of Wisconsin–Madison provide a tool kit for people struggling with pandemic stress.
It is clear the coronavirus pandemic is taking a significant emotional toll even on those without a SARS-CoV-2 infection.
The Kaiser Family Foundation Health Tracking Poll from July 2020 found that 53% of respondents reported pandemic-related stress negatively affecting their health.
The majority of those polled felt the worst was yet to come. Five months from that last sampling, the future remains uncertain even as the first coronavirus vaccines start to emerge.
"Traditionally, the focus in psychology research has been on treatment of mental illness,” says Christy Wilson-Mendenhall of the Center for Healthy Minds at the University of Wisconsin–Madison (UW–Madison) and a co-author of a new paper published in Proceedings of the National Academy of Sciences of the United States of America.
Struggling to cope with the pandemic, however, is not a matter of mental illness.
“We are hoping to broaden the conversation to advocate cultivating well-being at any stage, even when you are relatively healthy,” says Wilson-Mendenhall. “These skills help make us more resilient in moments like we are experiencing now.”
The study presents a four-part, self-taught program for mental well-being that can benefit anyone struggling with stress.
“It is really the ‘how’ of well-being,” Wilson-Mendenhall explains.
The 4 pillars of mental well-being
Wilson-Mendenhall and her colleagues — lead author Dr. Cortland Dahl and Dr. Richard Davidson, both of UW–Madison — have constructed a framework atop four pillars, or practices. They are well-regarded mental health skills that anyone can learn:
- awareness — a conscious focusing on one’s surrounding environment and senses
- connection — appreciation of others in one’s life, as well as compassion and kindness
- insight — an interest in self-knowledge and curiosity
- purpose — developing a clear sense of one’s values and motivations
Dr. Dahl says:
“There are qualities of a healthy mind that many people do not know are even trainable. We do not think of them as skills. Many of us have thought we are hardwired to be like this or that, but the reality is these qualities are much more trainable and malleable than we think. It is a very empowering view of the human mind — we can learn to be in the driver’s seat of our own mind.”
The researchers want their framework to be available to as many people as possible.
They look forward to healthcare professionals and researchers using the program in their own interactions with people who have a difficult time.
The research is published under a Creative Commons License, so it is freely available to any interested party.
By : Robby Berman
Fact checked by : Hannah Flynn, MS
Date : December 19, 2020
Source : Medical News Today
https://www.medicalnewstoday.com/articles/study-offers-a-mental-well-being-tool-kit-anyone-can-use
Here’s the first Africa-wide survey of the economic impact of COVID-19 on cultural industries
Arts and culture play an important role in all societies. They contribute not only to the social well-being of people but also to the social and economic development of countries. They generate incomes, as many case studies show, even if the level of informality of the sector in Africa tends to absorb that reality.
According to the United Nations Conference on Trade and Development’s report on creative economy (2018), the global market of cultural goods and services doubled from US$208 billion in 2002 to US$509 billion in 2015. An Ernst & Young study (2015) indicates that cultural industries in Africa and in the Middle East are worth US$58 billion in revenues, employ 2.4 million people and contribute 1.1% to regional GDP.
Like all economic sectors, cultural and creative industries globally have been negatively affected by the COVID-19 pandemic, specifically by the measures adopted by governments to limit the spread of the virus.
The impact has been well documented in advanced economies. However, data on the impact of COVID-19 on African cultural and creative industries is patchy.
According to Ernst & Young, the most lucrative of these industries in Africa are music, visual arts and movies. However, the low internet penetration holds back the rise of a promising sector such as online gaming. This in contrast with the high potential of the market. In fact, cultural policies are lacking or are not well implemented in many countries.
Using my experience in conducting an online survey in the Democratic Republic of Congo, I surveyed participants in the cultural and creative industries in six countries across four regions of sub-Saharan Africa.
A matrix of economic impact of COVID-19 included in my study reveals there are several factors explaining the harsh impact of the pandemic on the cultural industries in Africa. These range from levels of informality and the size of companies to the types of contracts used and the modes of production and consumption in the industries.
The method
I compared quantitative studies available in four sub-Saharan African economic regional communities in order to map the numbers. These are the Economic Community of West African States (Senegal), the Economic Community of Central African States (DR Congo), the East African Community (Kenya and Uganda) and the Southern African Development Community (South Africa and Namibia). Those countries are the only ones that had available data resulting from completed surveys at the time of writing the research.
All of them were based on online surveys conducted during the various lockdowns that occurred between March and May 2020. Even if questionnaires were not the same in all countries, similar and recurrent entries offered a basis for comparison. They are, of course, early assessments as the pandemic continues.
The authorship of those studies is private (associations, firms, academics), except in South Africa with its South African Cultural Observatory, a public research centre hosted by the Nelson Mandela University.
Our research privileged quantitative data. Nevertheless, the qualitative data available – such as case studies – were mentioned. They have been produced by the Center for Strategic and Defense Studies of Ghana and by Circulador, a travelling research platform for lusophone countries (Angola, Mozambique and Cape Verde). An interactive map allows for visualising data.
Key findings
Financial losses (turnover) in the cultural and creative industries in Africa during the second quarter of 2020 vary significantly from one country to another. Figures range between US$134,360 for Uganda and US$1.49 billion for South Africa, respectively 0.002% and 1.7% as contributions to GDP. The combined turnover during the lockdown period of the six countries in which the online surveys were done comes to a total of US$1.5 billion.
The most affected subsector within the cultural industries in Africa was the performing arts – such as live music, dance, theatre and events. This is explained by the ban on gatherings in these countries due to the pandemic. The content subsector – audio-visuals, cinema, visual arts – came second.
The studies also shed light on the most profitable subsectors during this period. Digital media, online gaming, music and audio-visual content were able to be resilient. Their value chains – from creation to consumption – don’t require a high level of mandatory face-to-face interaction and effective use can be made of online tools.
Vulnerability
My study reveals that the vulnerability of African creative and cultural industries resulted mainly from five factors:
- The predominance of the informal sector (53.3% in Senegal, 51.7% in Namibia, 80% in Kenya, 35% in South Africa).
- The significant number of freelancers whose resources cannot withstand shocks (68% in Kenya). In Uganda, nearly 700 artists are affected out of 3,000 cancelled events.
- The very small size of companies (47% of companies in DRC have between one and five employees; 80% have between one and 10 in Kenya). This is a further handicap because bigger companies are likely more resilient due to better access to financial, human and technological resources.
- The prevalence of part-time jobs and short-term contracts (58% of companies in Kenya have part-time jobs).
- The mode of production and distribution requires a high level of human interaction, especially for the visual arts (such as painting and photography).
Beginning of a journey
The pandemic has not only negatively impacted the creative sector in Africa, but it has also exposed its shortcomings.
To boost the cultural industries’ contribution to national economies, it is important to first conduct regular field studies to map the sector for oriented and efficient public and private interventions to enable the sector to recover from the setback of COVID-19. Governments have an important role to play in this regard.
It is well worth creating safer legal and business frameworks that will enable creative industries to operate more efficiently. Sound cultural policies along with implementation plans are key towards achieving this goal.
By : Ribio Nzeza Bunketi Buse (Associate Professor, University of Kinshasa)
Date : December 28, 2020
Source : The Conversation
https://theconversation.com/heres-the-first-africa-wide-survey-of-the-economic-impact-of-covid-19-on-cultural-industries-151400
Coronavirus new variant – genomics researcher answers key questions
A new variant of SARS-CoV-2, the virus which causes COVID-19, is thought to be driving increased transmission of the disease in parts of the UK. The government has placed some regions including London under new, stricter coronavirus restrictions, known as Tier 4. People in Tier 4 areas will not be able to gather with anyone outside their household for Christmas, while those in the rest of the country can only gather on Christmas Day itself.
Boris Johnson, the prime minister, and his chief scientific advisors said that the new variant could increase transmission of COVID-19 by as much as 70% and increase the R or reproduction number by 0.4%.
What’s the significance of this new discovery? The Conversation asked Lucy van Dorp, a microbial genomics researcher and an expert in the evolution of pathogens, some key questions about what we know at this point in time.
What do we know about this new variant?
The new UK variant, known as VUI–202012/01 or lineage B.1.1.7, was first identified in the county of Kent on September 20. Matt Hancock, the health secretary, first announced the existence of the variant on December 14; it was subsequently confirmed by Public Health England and the UK’s COVID-19 sequencing consortium.
The variant carries 14 defining mutations including seven in the spike protein, the protein that mediates entry of the virus into human cells. This is a relatively large number of changes compared to the many variants we have in circulation globally.
To date, genetic profiles – or genomes – of this variant have been largely sequenced and shared from the UK but include some in Denmark and two cases in Australia. There have also been reports of a case in the Netherlands. These countries all have very large genome sequencing efforts and it is very possible that these observations do not reflect the true distribution of this variant of the virus, which could exist undetected elsewhere. We will know more as more genomes are generated and shared.
Thanks to the efforts of data sharing, genomic surveillance and COVID-19 test results in the UK, it seems that this variant is now starting to dominate over existing versions of the virus and that it may be responsible for an increasing proportion of cases in parts of the country, particular in regions where we also have rapidly expanding case numbers.
It is always very difficult to disentangle cause and effect in these cases. For example increases in the appearance of certain mutations can be due to viral lineages carrying them rising in frequency just because they happen to be the ones present in an area where transmission is high, for example due to human activities or choice of interventions.
Though this is still a possibility, there are clearly enough concerning observations so far for this variant to warrant very careful characterisation, surveillance and interventions to curb transmission.
Is it more dangerous?
Chris Whitty, the chief medical officer, stated clearly that there was no evidence to date that this variant alters disease severity, either in terms of mortality or the seriousness of the cases of COVID-19 for those infected. Work is underway to confirm this.
How do virus mutations happen?
Mutations are a natural part of virus evolution. In the case of SARS-CoV-2, these mutations may arise due to random errors during virus replication, be induced by antiviral proteins within infected people, or via genetic shuffling – known as recombination. Though signs of recombination are not currently detected in SARS-CoV-2.
Most viral mutations are expected to have no impact. For example, when our team assessed individual mutation replacements in more than 50,000 genomes from the first wave of the pandemic, we detected none that significantly altered viral fitness – the ability of the virus to survive and reproduce.
However, every so often a mutation, or in this case a particular combination of mutations, may strike lucky and offer the virus a new advantage. Viruses carrying these combinations of mutations may then increase in frequency by natural selection given the right epidemiological environment.
Where did the variant come from?
Right now, we don’t know. To date, scientists have not identified any closely related viruses to support the theory that the variant had been introduced from abroad. The patterns of mutations observed are more supportive of an extended period of adaptive evolution most likely in the UK based on current data.
Similar patterns of mutation to these have been observed in the evolution of SARS-CoV-2 in chronically infected patients with weaker immune systems. The current hypothesis is that such a scenario of chronic infection, in a single patient, may have played a role in the origin of this variant. This will continue to be investigated.
How many variations of SARS-CoV-2 have we found?
There are many thousands of lineages of SARS-CoV-2 which differ on average by only a small number of defining mutations. It remains true that SARS-CoV-2 currently in global circulation have little genomic diversity. Subtleties in the mutations carried in different lineages can, however, be very useful for reconstructing patterns of transmission.
As an example, work early in the pandemic used lineage assignments to identify at least a thousand introductions of SARS-CoV-2 into the UK.
Why is this one different?
It is important to note that many of the mutations defining the UK variant have been observed in SARS-CoV-2 before and even sometimes quite early in the pandemic.
Yet the UK variant, or lineage, is defined by an unusual number and combination of mutations. One of these mutations, N501Y, has previously been shown to increase binding of the virus to receptors in our cells. N501Y was first sequenced in a virus in Brazil in April 2020 and is currently associated with a SARS-CoV-2 variant also rising in frequency in South Africa – an independent lineage from B.1.1.7 that is also warranting concern.
The particular deletions identified in the spike protein of B.1.1.7 have appeared in multiple other lineages of the virus at increasing frequency and are also observed in chronic infections where they may alter antigenicity - recognition by immune antibodies. These deletions may also be associated with other mutations in the binding region of the coronavirus spike protein, including those observed in infections among farmed mink and a mutation shown to play a role in the virus’s ability to evade the immune system in humans. B.1.1.7 also harbours a truncated ORF8 gene, with deletions in this region previously associated with decreased disease severity.
The functional effect of these mutations and deletions, particularly when in the combination reported in B.1.1.7, are still to be determined. The high number of mutations and the recent increase in prevalence of this particular variant, together with the biological relevance of some of the mutation candidates, emphasises the need for in-depth study.
What does this mean for the vaccine?
At the moment we don’t know. Though we should be reassured that vaccines stimulate a broad antibody response to the entire spike protein, so it is anticipated that their efficacy will not be significantly hampered by mutations. This is already being tested.
However, there is an increasing body of evidence that other species of seasonal coronaviruses exhibit some ability to escape immunity over longer time periods.
It is therefore conceivable that we may reach a point where we are required to update our COVID-19 vaccines, as we do for influenza, to reflect the variants in circulation at the time. It’s too early to say if this will be the case now, but extensive genome sequencing, data sharing, and standardised reporting of variants will be vital to inform these efforts.
By : Lucy van Dorp (Senior Research Fellow, Microbial Genomics, UCL)
Date : December 20, 2020
Source : The Conversation
https://theconversation.com/coronavirus-new-variant-genomics-researcher-answers-key-questions-152381
A moment in time: COVID, localisation and the Pacific
As COVID-19 was declared a pandemic and international travel restrictions, border closures and lockdowns ensued, large numbers of expatriate aid workers returned to their home countries. This significant change in the demography of the aid industry in many countries has led to a shift in roles for international, national and local actors in humanitarian and development work.
So, what are we witnessing? This period is a unique moment in time, one that presents challenges and opportunities for locally led humanitarian response and development. A number of initiatives have sought to explore these dynamics, and to understand what this means now, and what it could mean in the future.
Following Tropical Cyclone Harold hitting the Pacific in April 2020, Australian Red Cross, together with Fiji and Vanuatu National Red Cross Societies, developed a case study that examined the changes to the nature of the emergency response brought about by the COVID experience. The study explored how COVID had impacted on usual ways of working and shifted the modus operandi of international responses. Several significant shifts occurred – local Red Cross actors found themselves with more leadership space and were highly influential and visible in leading and setting national priorities, greater local procurement took place (despite a primarily internationally driven supply chain), and there was an increase in direct funding to the local National Societies.
Local actors had more space and prominence – everyone was looking to the Red Cross to partner with them. Local humanitarian actor, Vanuatu
No turning back: local leadership in Vanuatu’s response to Tropical Cyclone Harold, conducted in partnership by the Vanuatu Association of NGOs and Humanitarian Advisory Group, also outlined key shifts from previous cyclone responses, such as increased local leadership and altered role for international actors in remote support.
COVID-19 has restricted a lot of international experts to step in and help, forcing us to do things within the country capacity. As much of a struggle as it is, this is a step forward for our country. Local humanitarian actor, Vanuatu
Other initiatives such as the Pacific Resilience Partnership Mapping Localisation Survey sought to explore key localisation areas, and the impacts of COVID-19 across development and humanitarian sectors in the Pacific. A strong emerging perception from the survey was that the impacts of COVID-19 would strengthen locally led response due to the reduced presence of international actors.
The TWG [Technical Working Group] intends to utilise the data from the survey to map out how it will support the various actors through a collaborative approach. It is about extending our network whilst at the same time providing an avenue where we can leverage resources and expertise to assist one another in the midst of this pandemic. The TWG will ensure that we utilise the expertise that we have within the region to support one another. That is localisation in action. Josaia Jirauni Osborne, Deputy Director, Pacific Islands Association of NGOs (PIANGO)
There are also changed ways of working and dynamics in relationships, due to less international presence and a shift in how international actors are working with national and local organisations. La Trobe University’s Institute for Human Security and Social Change, with partners such as the Australia Pacific Training Coalition (APTC) and others, have been exploring organisational adaptations and the impacts on relationships.
We reached a point where the expats were asked to return at which point the local staff were presented with this opportunity to make things happen. Not only in terms of contributing to the decisions around key functions of the program but more importantly to constructing the response to COVID and how we would impact our core functions. This forced the local team to really take ownership of the situation because we understood the context, had the relationships with key stakeholders, we knew the influences. Jovesa Saladoka, APTC
Common threads
It turns out that there are emerging common threads across these various research initiatives. A window of opportunity: learning from COVID-19 to progress locally led response and development think piece explores these emerging findings, poses important questions for international humanitarian and development actors to consider in their work across the region and suggests that the sector has a critical window of opportunity to learn and build on the opportunity for positive change.
First, new spaces for local leadership have emerged. National actors report that the reduced physical presence of international aid workers has enlarged their space for local leadership and seen them exercise greater influence over decision-making.
Second, remote support has worked where strong relationships and trust were already in place. Some 70% of the TWG survey respondents outlined an increase in remote support (i.e. online mentoring and technical assistance). Many interviewees note that it is useful to have assistance available at the end of the phone, or short-term assistance, rather than creating the relationships of dependency which come from technical assistance being based full-time in Pacific offices.
Third, local humanitarian organisations report receiving more funding; however, most funding still goes through international mechanisms.
From where I see it, the situation may have contributed to a great opportunity to lead, coordinate and decide on what they see best, however it all falls back to funding … even if there has been increased funding there is still remote control on how it should be spent. National representative, Vanuatu
A total of 66% of national and local actors in the Pacific report receiving an increase in funding in the wake of COVID-19, and 61% of national or local actors report new partnerships with other organisations. However, there is little change to a system where the amount of direct funding to local organisations remains at around 2% of total humanitarian funding globally, despite the 2016 Grand Bargain commitment of 25%.
Making the most of the window?
Localisation is a journey and until it is supported 100 per cent by the international actors, it will remain just there – local actors doing the implementation and the international actors coordinating and chances not given to local actors to exercise their powers and their expertise in how to respond to natural disasters. National representative, Vanuatu
As the sector shifts back into a COVID-normal state, international actors will begin to return to the Pacific. There is a window of opportunity to adopt new practices which learn from and build on the positive adaptations made over the past year. This opportunity might be missed in the rush to return to ‘normal’. In all sectors, questions are being asked about how the COVID-19 pandemic has changed ways of working for the better (while recognising that some have changed for the worse) and therefore what features need to be retained.
By : Josaia Jirauni Osborne, Linda Kenni, Shirley Abraham, Josie Flint, Fiona Tarpey, Chris Roche
Date : December 17, 2020
Source : DevPolicy Blog
https://devpolicy.org/a-moment-in-time-covid-localisation-and-the-pacific-20201217/
Coronavirus: why is eastern Europe’s second wave so much worse than its first?
Eastern Europe was praised for being exceptional during the first wave of the pandemic. By introducing very strict prevention measures early on, countries in the region had significantly fewer COVID-related deaths than their western European counterparts.
Some argued that this was because of economics: that eastern European countries locked down early because they feared their economies would not be able to handle many people getting sick. Others suggested this eastern European exceptionalism could be explained by culture, with success in limiting the first wave being down to a mentality of fear and readiness to follow harsh rules stemming from the communist era.
But if these factors were at play in the first wave, they haven’t had the same effect in the second. Eastern Europe’s pandemic experience has been dramatically different this autumn. All countries in the region have seen significant increases in cases and deaths. Here, we take a look at why this has happened.
A head start in the first wave
One thing is clear: eastern Europe exited the first wave at the end of June in much better shape than western Europe. Adjusting for population size, both cases and deaths were substantially lower in the east, as shown in this comparison of the COVID-19 death rate in the two regions.
We can also compare how restrictive the two regions’ disease-prevention measures were during the first wave using the Oxford COVID-19 government response tracker (OxCGRT). This tool measures the stringency of efforts to control the virus on a scale of 0-100, with 100 being the most restrictive. We can see from the next graph that, at the same time in the spring, the two regions introduced measures that were similarly strict.
However, if we look back at the death rates of the two regions in the graph above, it’s clear that eastern European countries introduced restrictions when experiencing far fewer cases and deaths. Therefore, the simplest explanation for why eastern Europe initially fared much better is that it had a head start. Countries in the region imposed strict measures while being relatively mildly affected, whereas western countries waited until things got bad.
This shows that eastern European countries took the opportunity to act quickly.
Squandering the spring gains
When we turn to the second wave (starting around September and ongoing), we’re faced with the opposite question: why did eastern European countries not act in spite of rapidly rising infections and deaths?
Eastern European death rates overtook those in the west in early October, but restrictions in the region – which had eased after the first wave – still lagged behind controls reintroduced in the west. Look again at the second graph above. It shows that in between the two waves, the east relaxed its measures further than the west, and was then less eager in reimposing them. Eastern Europe squandered its spring gains and then repeated the mistakes made by the west in spring: waiting until cases and deaths are out of control before imposing controls.
What explains this reluctance to reintroduce restrictions? One explanation might be that these countries are victims of their own success. Eastern Europe contained the virus so successfully in spring, it didn’t experience the horrific hospital scenes seen in northern Italy, for example. This may have produced scepticism about the severity of the pandemic. Pandemic fatigue is present across the entire continent, and may be especially present in the east, where some people may have felt that they went into a lockdown for nothing.
Not all in the same boat
Importantly, however, there have been major differences within eastern Europe too. Up until the beginning of November, the spike in the death rate was largely driven by the Czech Republic. Cases and deaths have not been spread evenly across the region.
If we look at the stringency of control measures, we can also see that not all countries acted in the same way. The Czech Republic acted very late, for example, imposing stricter measures at the end of October, even though cases and deaths had been soaring upwards during the month. Neighbouring Slovakia, on the other hand, imposed stricter measures despite having far fewer cases and deaths. It seems that at least some countries in the region have learned their lessons.
Understanding why eastern European countries chose to respond differently during the second wave is complicated, though.
For example, differences in economic strength could explain why the relatively richer Czech Republic waited to reintroduce restrictions (thinking it could bear the brunt of a high number of infections), but this doesn’t account for the relatively poorer Romania’s decision to do the same.
Politics might provide a hint: the Czech Republic held regional elections in October, while Romania voted in local elections in September and is about to vote in national elections in December. Electoral politics could explain the reluctance of the two countries to enter another lockdown – with politicians seeing it as an unpopular measure that would also delay elections.
But one explanation that can probably be ditched is the culture argument mentioned previously. Even in countries where governments reintroduced relatively strong restrictions in October, such as Slovenia and Lithuania, infections and deaths have remained high throughout November – suggesting low compliance with the rules.
By : Tamara Popic (Max Weber Fellow in Social and Political Sciences, European University Institute)
Alexandru D Moise (Max Weber Fellow in Social and Political Sciences, European University Institute)
Date : December 2, 2020
Source : The Conversation
https://theconversation.com/coronavirus-why-is-eastern-europes-second-wave-so-much-worse-than-its-first-150430
When culture clashes with Covid-19
MIT panelists examine the roles of social norms in countries’ differing responses to the coronavirus pandemic.
In China, wearing masks during an epidemic is a readily accepted practice — unlike the situation in, say, the United States or some European countries, where the issue of mask-wearing is revealing civic and political fault lines. To what extent are these differences attributable to the “culture” of each country? And how much have widespread social norms affected the responses of different countries during the Covid-19 pandemic?
Those were among the leading questions driving an MIT public forum on Tuesday, as leading scholars from the Institute examined the connections between social practices and national responses to the pandemic. Although, to be sure, it is difficult to generalize about national cultures, as the scholars noted.
“Most scholars these days are extremely reluctant to ascribe outcomes to culture,” said MIT political scientist Chappell Lawson, who moderated the event.
Still, Lawson added, during a time of a global public health crisis, it is at least possible to ask how social practices have fed into the varying responses around the world: “The basic question related to culture is how do the habits and mindsets of a group of people — what Alexis de Tocqueville once called morays — affect what people do in the public sphere. In this case, how do those beliefs and norms affect what different countries did in response to the emergence of the SARS-CoV-2 virus?”
Under these terms, “Some of the choices the governments have made may be a product of culture,” added Lawson, an associate professor in MIT’s Department of Political Science, who also directs MIT International Science and Technology Initiatives (MISTI).
Yasheng Huang, a professor of management at MIT, contended that cultural effects are real and significant, even if they can be difficult to quantify.
“It’s hard to study [culture], it’s hard to measure, but we should try harder, rather than saying it doesn’t matter,” said Huang, who is the Epoch Foundation Professor of International Management at the MIT Sloan School of Management and faculty director of the MIT-China program. “I think culture matters tremendously in terms of this response, as well as the outcome.”
Huang added: “One way to think about culture is, people act on certain norms without thinking about those norms every day.” That includes, yes, mask-wearing.
“In East Asia, nobody questions the value of wearing masks, and people began to wear masks very early on, without the government mandate,” says Huang, noting that “people in Hong Kong began to wear masks on their own in late December and early January.”
For culture to connect with policy, however, there needs to be public trust in government, said political scientist Suzanne Berger, a longtime expert on French politics, who contrasted France’s faltering public response with Germany’s greater success.
“In observing the cases of France and Germany, what we can recognize is that the most vital national supply is trust,” said Berger, the John M. Deutch Institute Professor at MIT. “Everything that’s involved in dealing with Covid, contact tracing and tracking, testing, all these really depend on trust, and that’s what’s been sadly depleted in the French case.”
The discussion, titled “When Culture Meets Covid-19,” was the latest public panel from MIT’s Starr Forum, an event series hosted by the Center for International Studies.
Trustbusting
To see why culture and trust matter so much in the pandemic response, Berger suggested, consider that, in material and institutional terms, France would appear to be well-situated to deal with a pandemic.
“I thought that Covid was exactly the kind of crisis that France should excel in managing,” said Berger, noting that it has a highly regarded national health service, significant medical research laboratories, and a strong central government.
Moreover, Berger added, referencing the work of French sociologist Michel Crozier, “The French are very reluctant to observe the authority of peers … so one should have anticipated that the French would feel right about [a] national authority making the rules about masks, social distancing, and testing.”
Instead, Berger noted, the French response has stumbled from the start. France had destroyed a large portion of its mask stockpile prior to 2020; the ensuing shortage led to mixed messages about mask-wearing, while controversies also erupted about therapeutics. As a result, Berger noted, just 39 percent of people in an April poll claimed they had confidence in the government’s ability to handle the crisis, down from 55 percent in mid-March.
“The polarization which we’ve seen divide the United States over how to deal with Covid took form in France, too,” Berger said.
Those kinds of divisions are evident in a variety of other countries, noted panelist Peter Krause PhD ’11, an associate professor of political science at Boston College and a Middle East expert, who talked about the situation in Egypt, Jordan, Israel, and Lebanon. As different as those countries all are, Krause noted, the reaction to pandemic policies varies among social, ethnic, and religious subgroups: “It’s not just country-wide, but within each country … you see these legacies of a lack of trust in the government,” Krause said.
Techno-cultures?
The situation in China is quite different, since China’s authoritarian rulers provide less room for public dissent. However, Huang said, he believes there is a tendency toward public compliance in the country that exists apart from the form of the government.
“It is not right to attribute the ability to lock down an entire city or province solely to the coercive power of the government, even thought there’s a lot of that as well,” said Huang. “We need to acknowledge the coercive power, but we also need to say that there is a cultural compenent in accepting … the government policy.”
More specifically, Huang added, in China, Japan, and South Korea “people there automatically think about technology as a solution,” making them relatively receptive to some of the initiatives used to battle the spread of Covid-19.
In response to audience questions, Huang indicated he was relatively comfortable generalizing about cultural similarities among different East Asian countries — but noted that we should distinguish between cultural affinities and the political responses of different countries, which have varied considerably. South Korea, which is a democracy, did not institute Chinese-style lockdowns, for instance, but developed an extensive system of early testing and contact tracing that has limited the spread of Covid-19.
In China, as Huang also noted during the question-and-answer session, the government response to the new virus faltered in its early stages, in late 2019, as officials initially did not acknowledge the potential severity of the new outbreak. In each country, though, Huang suggested that cultural norms have helped compliance with government actions.
“I think in the Chinese culture, and East Asian culture, there is quite a bit of trust,” Huang said. “Sometimes it’s not earned, sometimes it’s not deserved, but it’s there to begin with.”
One final difference between East Asia and the rest of the globe regarding Covid-19, he noted, is recent history, which has also shaped public attitudes significantly.
“One difference between Asia, and Europe and the United States is that Asia experienced SARS,” Huang said. “China experienced SARS, Hong Kong Experienced SARS, Taiwan experienced SARS, and that searing experience shaped the mentality,” informing public acceptance of a forceful Covid-19 response.
This changes everything?
During a question-and-answer session, the panelists were queried about what kinds of long-lasting cultural changes might arise from the Covid-19 pandemic, and they suggested a variety of possible lasting trends.
“Basically I think it’s going to be a shock that promotes nationalism,” said Berger. “That is, a desire for more protection from the state, a desire for closing up the borders, a desire for having more production take place within national boundaries.”
In the Middle East, Krause said, “I think the impact is going to be somewhat lessened because of the smaller number of cases, but … one of the key areas that you look at is social trust between different ethnic groups.”
Across countries, he added, “One of the things that I’ll keep an eye on is that, when you have pandemics like this, certain populations can be accused of being the carriers of the disease, and face greater discrimination going forward, so that can break down some of the bonds of social trust. That will be, potentially, one of the key legacies, if that happens.”
By : Peter Dizikes (MIT News Office)
Date : June 25, 2020
Source : MIT News
https://news.mit.edu/2020/when-culture-clashes-covid-19-0625
Coronavirus and securitization of migration in South America: The Venezuelan journey
The pandemic has deepened the vulnerability of Venezuelan migrants in South America, especially in Ecuador, Peru, Chile and Colombia.
The coronavirus pandemic has produced profound impacts worldwide, but some populations have been hit hardest, including migrants. This article analyzes how the pandemic has deepened the vulnerability of Venezuelan migrants in South America, especially in Ecuador, Peru, Chile and Colombia.
Since 2014, more than 5 million citizens have left Venezuela, mostly to neighboring countries. This scenario started due to the economic, political, supply and humanitarian crisis faced by the State. The government of Nicolás Maduro is accused of political persecution of the opposition and also of using the humanitarian crisis as a persecution tool. For those reasons, the Organization of American States (OAS) and the United Nations High Commissioner for Refugees (UNHCR) recommended recognizing Venezuelans as refugees under the 1951 Refugee Convention. Both organizations also stated that recognition could be achieved based on the wider criteria of the 1984 Cartagena Declaration on Refugees.
Securitization of migration in South America
This migration flow provoked different government responses across South America. Firstly, none of the regional countries has recognized Venezuelans as refugees under the Cartagena Declaration. Only a few were recognized under the 1951 Convention and on a case-by-case basis. In July 2019, Brazil became the first country in South America – and only thus far – to recognize Venezuelan migrants as refugees based on the wider criteria of the Cartagena Declaration. Thus, the regularization of Venezuelans occurred mostly on an ad hoc basis.
The high intensity of the migration flow and the proliferation of xenophobic discourses led to the adoption of securitization measures in three of the region’s States. Chile was the first to restrict the entry of Venezuelans. In April 2018, Chile – which already required Venezuelans to present a passport to gain entry– began to impose the 'democratic responsibility visa' on citizens of this nationality. This measure led to an increase in the number of Venezuelans in Peru, as many of them, unable to enter Chile, were “stuck” at the border.
As a result, in April 2018, Peru started to require passports from Venezuelans, with the exception of asylum seekers. On June 2019, Peru adopted another security measure and began to require a humanitarian visa. The same situation happened in Ecuador after Peru's newly imposed measures: many Venezuelans were "stuck" at the Ecuador-Peru border. In July 2019, Ecuador also created a humanitarian visa, which was required upon entry and also became mandatory for the regularization of Venezuelans already in the country, but was only available to those who had entered legally.
Visa and passport requirements are “no entry” measures created by the securitization of migration. These measures aim to reduce immigration under the guise of national security [i]. In the Venezuelan case, passports have become increasingly difficult to obtain over the past few years. Even though most countries accept expired passports, many people were never able to obtain them in the first place. Visa requirements restrict regular migration even further, as the application process involves — in addition to a passport — tax payments and documents which are difficult to obtain, like criminal records.
The existing migration corridor, from Venezuela to Chile, has been securitized, with the exception of Colombia. It is important to highlight that Peru, Ecuador and Colombia, in addition to being transit countries, are also destination countries. As is well documented in the literature, securitization measures do not reduce migration – but they do increase the vulnerability of migrants. In light of the new security measures, they are at the mercy of "coyotes" and have to risk their lives in dangerous ways. Once at their destination, these migrants are considered "illegal" and have no access to government assistance. Moreover, their irregular status makes them susceptible to exploitative conditions from employers and tenants. Thus, they mostly establish themselves on the informal market.
How does COVID-19 affect Venezuelan refugees?
The coronavirus pandemic added another layer to the issue. Many Venezuelans who lived in Chile, Colombia, Ecuador and Peru started to go back to Venezuela. A situation that was already difficult became more dire: Many Venezuelans lost their income, their houses and were starving. This situation caused what Espinoza, Zapata and Gandini called “mobility in immobility”, which describes the continued migration flows amid borders closures to contain the spread of COVID-19.
The regularization of Venezuelans in the countries to which they have moved is directly linked to the social issue. It is only once they are regularized that they can obtain local documents, which allows them to search for formal jobs. In addition, only regularized migrants are able to apply for government assistance, such as cash transfer programs for families living in a situation of social vulnerability. Examples include “Bolsa Família” in Brazil; “Chile Solidario”; “Programa Nacional de Asistencia Solidaria” in Peru; “Famílias en Acción” in Colombia; and “Bono de Desarrollo Humano” in Ecuador.
Despite being available to all citizens of their countries, these aids are not granted indiscriminately. Thereby, many migrants cannot rely on those government programs. Furthermore, even those who qualify for aid find themselves in a difficult financial and social situation as the amount is not enough to cover all expenses. This population also has greater difficulty in accessing education and health services. In addition, they face numerous obstacles to getting a formal job, especially in Brazil, due to the language barrier. However, even formal work does not guarantee a stable income for families, a situation which has worsened sharply during the pandemic[ii] .
Brazil has not adopted securitization policies like the previously discussed countries and there is no news of widespread repatriation. But this does not mean that the situation of Venezuelans in the country is any easier. In big cities, where the cost of living is even higher, people are being evicted from their homes and facing food insecurity. Although the government has made emergency aid available to people in situation of vulnerability, as with the cash transfer programs, not everyone who needs it is able to receive it. Moreover, the crisis caused a rise in unemployment, further aggravating the vulnerability of these populations.
In this context, the solidarity of those helping migrants and refugees comes into play. Venezuelans first seek help within their community, a network of friends and churches that often donate food, clothing, furniture, among other items. Mostly linked to the Catholic church, NGOs also help refugees and asylum seekers.
However, fundraising campaigns are enough. In light of the pandemic, specific public policies need to be put in place to address the situation faced by migrants and refugees — regardless of legal status — to prevent their rights from being further violated.
References:
[i] Gerard, A. (2014). The securitization of migration and refugee women. London: Routledge.
[ii] Jubilut, L. L. et al. (2020) Direitos Humanos e Covid-19: impactos em direitos e para grupos vulneráveis. Grupo de Pesquisa “Direitos Humanos e Vulnerabilidades” da Universidade Católica de Santos, Santos.
By : Mariana Almeida Silveira Correa and Mariane Monteiro Da Costa
Date : September 24, 2020
Source : Open Democracy
https://www.opendemocracy.net/en/democraciaabierta/coronavirus-securitization-migration-south-america-venezuelan-journey/
COVID-19 Is Widening Educational Inequalities for Children Around the World
In poor and developing countries, school closures can have a devastating impact on children.
Schools and families the world over are grappling with the challenge of educating children in a pandemic. Pushing children back into schools might increase the COVID-19 infection rate. But keeping them home could threaten their future too — particularly if they don’t have internet access.
Even in the wealthiest nations, the digital divide is widening inequality gaps, leaving many poor children behind. In the United States, nearly 17 million children lived in homes without high-speed Internet in 2018. While school systems there are rushing to close these gaps, millions of American children are still disconnected.
The problems in my country, Kenya, are much more severe. According to the latest UNICEF publication, just six percent of children have access to the internet in the eastern and southern Africa region.
Amongst the Kenyan children without internet access are vulnerable rural girls and boys with untold stories and dreams, whose hopes for the future remain in limbo. COVID-19 is particularly devastating for my country’s large orphan population, whose stories are already hidden in data and figures. Kenya has an estimated three million orphans, one third of whom lost their parents to another global pandemic, HIV-AIDS.
Education once gave these vulnerable children a glimpse of hope. But not now, with schools closed for the past six months, they’ve gotten used to the idea of no school calendar in 2020. Once again these children are having to live through a pandemic, their dreams left at the mercy of an unpredictable future, in remote rural villages, with weak education and other infrastructure.
One likely COVID-19 impact is a rise in teen pregnancies, since adolescent girls are without the safety net that schools provided. This gendered menace deprives young girls of the opportunity to further their education and attain their career goals. It also exposes them and their children to major health risks. According to the World Health Organization, “pregnancy and childbirth complications are the leading cause of death among girls aged 15–19 years globally.”
One pregnant 15-year-old, “Adelina” (not her real name), spoke about her predator with the community action team of the Rona Foundation, which supports rural widows and orphans.
“He bought me toilet paper and ng’ombe (a type of moisturizer similar to petroleum jelly that sells for 30 Kenyan shillings, or about 28 U.S. cents),” she said. “He threatened to kill me, if I ever told anyone.”
Adelina, who lost both of her parents and has been under the care of her aging grandmother, explained that the predator and her close relatives agreed to let the matter rest, with a promise that she would later be taken to live in the city with an aunt she has never met.
Similar stories are rampant across remote rural villages in Kenya, yoking even the bravest of feminist hearts.
“Prolonged closure of schools means a number of our girls will not have a chance of coming back to school” says Lawrence Otunga, Chairman, Trained ECD Teacher Association (TETA) Kenya.
What can be done? The Kenya Ministry of Education has tried to launch a “community-based” learning plan with classes in open places, but it has been blocked by a court order. Since then, government officials have issued contradictory statements as they struggle to come up with alternative plans.
While one can understand the complexity and the uncertainty of the moment, there is an urgent need to fast track key actions to safeguard further social and economic consequences on Kenyan society and the economy.
The government should partner with businesses and nonprofit organizations that have resources, networks, and access to remote villages. Implementing community-based learning through local grassroots organizations may be the way to make this alternative approach achievable at this point of the pandemic.
The Ministry of Education will also have to revive the now dead laptops for primary children project, with policies that provide remote learning opportunities at the pre-primary level that are vital now more than ever. To do one and not the other, means rural children will never be able to compete with their urban counterparts, and technology-enhanced teaching and learning will remain a mirage.
Besides digitalizing the syllabuses, there is a greater need to build capacities of teachers on e-learning, create e-learning labs in rural schools and community centers, and stabilize the electricity supply in far-fetched counties, or/and fund alternative energy sources to rural schools.
COVID-19 has revealed the desire for a creative and craft/talent economy besides classroom learning. So, as the government grapples with education challenges during and beyond this pandemic, there is a need to take little steps in reimagining the learning environments.
In the long term, there is also a need to involve more stakeholders to support ongoing efforts to replace our traditional system with one that focuses on core competences such as communication and collaboration, critical thinking and problem-solving, creativity and imagination, citizenship, digital literacy, learning to learn and self-efficacy.
Kenya’s challenges are extremely serious. But we are not alone. According to UNICEF, at least 31 percent of schoolchildren worldwide cannot be reached by remote learning programs, whether through the internet, TV, or radio.
The whole world will suffer from the lost educational opportunities for these many millions of children left behind.
Roseline Orwa is founder of the Rona Foundation, which supports rural widows and champions the protection and advancement of their rights, alongside orphan education, care, and support via the Rona Orphans and Widows Centre in rural Kenya. She is an Atlantic Fellow for Social and Economic Equity and an appointed Commissioned Expert with the Ministry of Labour and Social Services. She tweets at @roselineorwa
By : Roseline Orwa
Date : September 16, 2020
Source : Foreign Policy in Focus
https://fpif.org/covid-19-is-widening-educational-inequalities-for-children-around-the-world/
Graduate Student Experiences in the Midst of Multiple Pandemics
COVID-19 has exposed America’s fragile fault lines associated with economic and racial inequality. In Summer 2020, Contexts Magazine: Sociology for the Public assembled a special COVID-19 issue. We received over 200 submissions from 25 countries, publishing some of the ones that made it through editorial review on our website. After peer review, some of these articles will be featured in our Fall 2020 issue on Pandemics.
Continuing this work, we asked members of the Contexts Magazine Grad Team to write essays from the doctoral student experience about the difficulties of this moment. The Contexts Magazine Grad Team typically writes 300-word essays on recently published articles in top sociology journals. This time, however, we hear directly from them. We ask that you really read to listen. Doctoral students are dealing with multiple sources of stress: a shrinking job market, racial inequity in their Black and Latinx communities, parenting during a pandemic, serving as caregivers to older adults, and engaging in racial equity work in the academy – an institution they collectively feel has failed them. We applaud these students’ courage to speak out. Their words matter. Contexts Magazine aims to be part of the solution to create space to listen, think, and then act to truly respond to the concerns of doctoral students during these troubling times. To our academic colleagues, we hope you do the same.
– Rashawn Ray and Fabio Rojas
- “Is the Academy Equipped to Properly Center Equity?” by Teagan Murphy
- “Agonizing Questions From a Black Graduate Student” by Simone Durham
- “Black Graduate Students are Tired but Continue the Work” by Joey Jennings
- “Impossible Circumstances for Parents and Grad Students of Color” by Chandra Reyna
- “Who does the healthcare system truly care for during COVID-19?” by Genesis Fuentes
- “Starting a Doctoral Program in Abnormal Times” by Katelyn Foltz
By : Rashawn Ray and Fabio Rojas
Date : October 2, 2020
Source : Contexts: Sociology for the Public
https://contexts.org/blog/graduate-student-experiences-in-the-midst-of-multiple-pandemics/?_ga=2.14981109.237250915.1601819906-1798653950.1595136795
Men and Women Agree: During the COVID-19 Pandemic Men Are Doing More at Home
Men and Women Agree: During the COVID-19 Pandemic Men Are Doing More at Home. They Differ Over How Much, but in Most Households the Division of Housework and Childcare Has Become More Equal
A briefing paper prepared by Daniel L. Carlson (University of Utah), Richard J. Petts (Ball State University), and Joanna R. Pepin (University of Texas-Austin) for the Council on Contemporary Families.
For the past 30 years the gender revolution has proceeded at a snail’s pace. Some argue it has actually stalled. Relationship quality and stability now appear greatest when heterosexual partners are equals, and some evidence shows that couples are increasingly likely to share domestic labor. Yet the proportion of couples who achieve egalitarian arrangements remains low relative to the proportion of adults who value gender equality. And now, as the COVID-19 pandemic rages, some fear the gains of the gender revolution will be erased. Recent surveys commissioned by the New York Times and USA Today appear to confirm such fears, suggesting that during the pandemic women continue to shoulder the majority of housework and childcare, and now also do the majority of homeschooling too, despite men’s claims to the contrary.
A focus on homeschooling as an emergent and pressing issue is understandable, given the way this task may exacerbate inequalities at home. But how partners divide the responsibilities for educating their children during the pandemic may tell us little about the future of gender equality once the pandemic ends, since homeschooling is temporary for most parents. When we examine trends in the division of those housework and childcare tasks that have been in the process of renegotiation for decades, the patterns provide evidence of more egalitarian progress.
A glass half full or half empty? Most women still do more at home than men, but many men are doing more than before the pandemic — and very few (if any) are doing less
Our survey[i], an online non-probability sample of parents (n = 1,060) in different-sex couples, conducted in mid-April, assessed divisions of labor during the pandemic and compared them to how couples divided labor before it began. Our results[ii] suggest a more hopeful scenario than those implied by the headlines: According to both men and women, men are doing more housework and childcare during the pandemic than before it began, leading to more equal sharing of domestic labor. Moreover, given the conditions under which men are doing more, there is potential that these changes may persist after the pandemic ends.
Though homeschooling falls largely on the shoulders of women, our results indicate that for the majority of men and women (approximately 60 percent), time in domestic labor has not changed since the beginning of the pandemic, even accounting for helping children with homework. This is because time in some tasks like transporting children, attending children’s events, organizing children’s schedules/activities, and grocery shopping (for women, at least) have declined dramatically or stopped altogether.
Men and women differ in their reports of who does more domestic work; the truth is likely somewhere in the middle.
One of the most provocative findings in the NYT and USA Today surveys is the discrepancy between men’s and women’s reports of who is doing what in the household. For example, in the NYT story, 80 percent of women report doing the majority of homeschooling right now. Yet 45 percent of men also claim to be doing most of the schooling, while only three percent of women report their male partners as the primary educator. Like the Times, we find that most women (70 percent) report being primarily responsible for homeschooling during the pandemic, but we find a much smaller gender gap in men’s and women’s assessments of men’s responsibilities for schooling: 20 percent of men say they are doing the online educating while three percent of women say their male partners are largely responsible. Discrepancies between the estimates in the two studies may be the result of sampling variation or differences in question wording – the NYT asked about homeschooling children or helping with distance learning – that may influence responses.
Men and women also differ in their reports of how much housework and childcare each is doing, although the differences are not as large as over the homeschooling question. The NYT story suggests that women’s estimates are more accurate than men’s. But it is not at all clear that men exaggerate their time use more than women in surveys or fail to notice their partners’ time use more than women do (Bianchi et al. 2000; Kamo 2000; Lee and Waite 2005; Yavorksy, Kamp-Dush, and Schoppe-Sullivan 2015). In an appendix to this report, we discuss why we use both men’s and women’s reports to construct estimates of the division of domestic labor during the COVID-19 pandemic – an approach we argue is ultimately conservative. Nonetheless, even if we rely only on women’s reports, the story from our data on how the pandemic has changed domestic labor is the same: Men are doing more housework and childcare since the pandemic began, and this has led to an increase in egalitarian domestic arrangements.
When we focus on the housework and childcare tasks that couples were dividing before the pandemic, we find that among couples where the division of tasks has changed, it has changed in an egalitarian direction. Indeed, in no situation — and in no type of family, whether dual-earner where both are working full-time, dual-earner where someone is working part-time, single earner, or both unemployed — did we find that the division of tasks became less likely to be shared.
Considering both men’s and women’s reports, we see that prior to the start of the pandemic, 26 percent of parents reported sharing routine housework[iii] relatively equally[iv] with their partner, 41 percent reported sharing care for young children[v] relatively equally – although physical childcare and the mental load of organizing children’s lives were by and large mother’s responsibilities — and 45 percent reported sharing care of older children[vi]. A little more than a month after the start of the pandemic, 41 percent of parents reported sharing housework with their partners – a significant 58 percent increase — while the percentage of partnered parents reporting equal sharing care of young and older children also increased significantly, to 52 percent and 56 percent respectively. The proportion sharing in the care of young and older children grew by 27 and 24 percent respectively, driven by increases in equal sharing of physical care, monitoring, reading, and organizing children’s activities.
We find similar evidence of change when we restrict analyses to women’s reports only. Only one-in-six women (16 percent) reported sharing housework with their partners prior to the pandemic, compared with more than one-in-four (27 percent) who reported sharing it during the pandemic. As for childcare, 28 percent of women reported sharing care of young children relatively equally prior to the pandemic while 34 percent reported sharing it equally during. For older children, women’s reports of equal sharing grew from 29 percent to 42 percent.
The increase in egalitarian arrangements is largely the product of men’s doing more. Forty-two percent of fathers reported an overall increase in housework time, 45 percent reported more time in the care of young children overall, and 43 percent reported more total care of older children. Many mothers also reported that their partners increased their total time in housework (25 percent), care of young children (34 percent), and care of older children (20 percent). Nonetheless, mothers are significantly less likely than fathers to report that fathers have increased their time in housework or childcare. Men and women who report that fathers increased their time in housework and childcare also widely report that they were sharing housework (69 percent) and childcare (76 percent) responsibilities equally with their partner during the pandemic or that the men were doing the majority.
Consistent with past research (Kamo 2000; Lee and Waite 2005), though men and women disagree on men’s time, there was no such disagreement regarding mother’s time. More than one-quarter of both fathers and mothers reported an increase in mothers’ time in housework and childcare. The women most likely to increase their time in childcare and housework were the ones who were already responsible for the majority of such work before the pandemic. Parents also agree that between 11-16 percent of mothers and 6-8 percent of fathers decreased their overall time in domestic work. This might be because some tasks are just currently obsolete.
We still don’t have an egalitarian utopia
Families are sharing domestic labor more equally since the start of the COVID-19 pandemic. That is not to say, however, that the pandemic has created an egalitarian utopia in households. Indeed, although conventionally gendered divisions of housework and childcare have become less common since the beginning of the COVID-19 pandemic, many mothers continue to find themselves in these arrangements. Of the mothers who continued to be primarily responsible for domestic work during the COVID-19 pandemic, roughly one-third increased their time spent in housework and care of children during the pandemic. Moreover, 70 percent are also solely responsible for educating their children. Consequently, among families that have not moved toward more egalitarianism, domestic work for mothers has become even more time-intensive.
The COVID-19 pandemic has disrupted every aspect of Americans’ daily lives. Stay-at-home orders in nearly every state, along with the closure of schools, childcare centers, and non-essential businesses, have placed immense strain on families, suspending important care supports and demolishing barriers between work and family roles. Our findings demonstrate that the COVID-19 pandemic has both exacerbated and reduced gender inequalities in the division of domestic labor. For women who continued to shoulder domestic work during the pandemic, housework and childcare responsibilities have become much more arduous. Not only are these women spending more time in classic tasks, but homeschooling has also been added to their plates. Nonetheless, though roughly half of women are doing most of the housework and childcare right now, according to our estimates another half of women are not. Among a sizeable number of families, the burden of domestic responsibilities has become more equal as fathers have increased their contributions to housework and childcare.
Will the trend towards egalitarianism last beyond the crisis?
A central question is whether fathers will continue their domestic contributions once the pandemic passes. The signs, we think, are encouraging. Research shows that many couples fail to craft egalitarian divisions of household labor in part due to unsupportive workplace-family policies (Pedulla and Thébaud 2015). The COVID-19 pandemic has eliminated some of the structural barriers to sharing domestic work – particularly for men – since many adults are now working from home. The pandemic has demonstrated that many jobs can be done remotely. To the extent such arrangements increase, this may create greater egalitarianism, because recent evidence from before the pandemic shows that men who work from home share more equally in domestic labor (Carlson, Petts, and Pepin 2020). However, whether men and women will continue to have schedule flexibility or the ability to work from home as employers re-open is unknown.
Nonetheless, just the experience of having heightened responsibilities for housework and childcare during this time bodes well for men’s continued involvement in housework and childcare. As research on paternity leave demonstrates, men who take leave, especially extensive leave (e.g., two months), continue their involvement in housework and childcare over the long-term even after returning to work (Petts and Knoester 2018; Bünning 2015). The longer the pandemic lasts, the more hardships most of us will experience. But perhaps in the aftermath the patterns of domestic involvement men are establishing now will become a new normal.
+++
FOR MORE INFORMATION, PLEASE CONTACT:
Daniel L. Carlson / Associate Professor / Department of Family and Consumer Studies / University of Utah / [email protected].
Richard J. Petts / Professor / Department of Sociology / Ball State University / [email protected].
Joanna Pepin / Postdoctoral Fellow / Population Research Center / University of Texas – Austin / [email protected].
LINKS AND ABOUT:
Report: https://contemporaryfamilies.org/covid-couples-division-of-labor/
Press Advisory: https://contemporaryfamilies.org/covid-couples-division-of-labor-advisory/
Date : May 20, 2020
Source : Council on Contemporary Families
https://contemporaryfamilies.org/covid-couples-division-of-labor/
Universities are being forced to lie about being COVID safe
Universities know they will become infection hot-spots. But shutting before the government tells them to will leave them bankrupt.
As the COVID-19 rate soars, universities are due to welcome students back over the next few weeks. Boris Johnson has warned students not to gather in groups of more than six. This is good advice, with the slight problem that it won’t apply to either their seminar teaching or to those with whom they share their accommodation, which is where they will spend most of their time. Students and lecturers, and their respective unions NUS and UCU, are deeply worried that universities are unsafe, views that are supported by scientists from both the government’s own advisory group, SAGE, and scientists from Independent-Sage. UCU argue that teaching online is the only way to prevent unnecessary deaths. So what do universities themselves think?
Officially the line from UUK, the organisation that represents university management, is that institutions will be COVID-secure. Unofficially, something quite different has been acknowledged. Universities know that they are likely to spread COVID-19 by bringing students onto campus, but they also know that without this they will go bust.
The radical changes made to shift Higher Education funding from the taxpayer to student fees has done more than turn education into a commodity. It has also made universities financially vulnerable to such an extent that they cannot survive without the money from student fees and accommodation. I was recently in a meeting in which a member of Senior Management at my institution stated explicitly that the university would be in serious financial trouble if the students did not return. Incredibly, this person also admitted that it was ‘inevitable’ that there would be an outbreak of COVID-19 as a result of campus reopening. It was made clear in the meeting that this information was confidential and should not be shared with the public. The position of universities is publicly to claim that they are safe, but privately to acknowledge that this is impossible.
It will be financially ruinous to many institutions if the students don’t come back. It will be a quite different thing, however, if the students return and then are locked down in campus accommodation because of a COVID outbreak. The intention, then, is to lure students to campus by pretending that they will be safe and then, when an outbreak hits, to go online, as has already happened at dozens of institutions in the USA. Perhaps the biggest irony is that large numbers of university students moving around the country is risking another national lockdown, wrecking the economy for the second time in a year.
Why would universities do this rather than simply switch to online teaching now? The reason is simple. If an institution decides on its own to not give students what they have been promised (i.e face to face teaching) then it will face action from the Office for Students for failure to deliver the ‘product’ to consumers. The consequences would be a mass return of tuition fees and financial ruin. But if a university is forced by a local or national lockdown to go online, they will not have to pay this money back. And of course, if students are locked down after they have arrived on campus, they will also be paying for their accommodation, which is a vital revenue stream. Universities know that the above situation is likely, even inevitable. They know they are lying to students about campus being COVID-safe. It is important that students know this too.
The position of universities is fraudulent and utterly immoral: they are prepared to let people get ill and even die to keep themselves afloat. But perhaps we should not be too harsh on individual institutions, for really the problem is the system itself. If it is financially impossible for Higher Education to keep students and staff safe then something has gone badly wrong with our funding model. The consumerist system of Higher Education is leading us down a path that will inevitably lead to additional deaths. We need a radical rethink. University research provides public benefit and so it should be paid for, as schools are, through public taxation, progressively tiered so that the rich pay the most. Giving universities financial stability is the only way to ensure that they are not forced into a corner where they choose their own survival over that of their students and staff.
The author is a staff member at a university in England.
By : Anon
Date : September 10, 2020
Source : Open Democracy
https://www.opendemocracy.net/en/universities-are-being-forced-lie-about-being-covid-safe/
Why COVID-19 Cases in Europe Are Surging Back to March Levels — What This Means for the U.S.
- COVID-19 cases have risen to March levels in many European countries, and new restrictions are being imposed.
- Experts say the fact Europeans usually take vacations in August and go to a handful of destinations is one factor for the spike.
- They also note that schools have reopened, and that also has an effect.
On March 31, with the still relatively new coronavirus shutting down much of Europe and forcing people to stay inside their homes, the number of reported daily new cases in France peaked at nearly 7,600.
That number gradually declined from then on. Over the spring and summer, social and economic activity in France and much of Europe gradually returned as people took new precautions to prevent the spread of COVID-19.
Then it started inching back up.
On Aug. 28, reported daily new cases in France surpassed the March record. A week later, there were nearly 9,000 new cases in 1 day.
The new spike there echoes what’s been happening in Spain, the United Kingdom, and several other European nations in recent weeks.
In the United Kingdom, new lockdown restrictions are being implemented next week.
What’s happening in Europe — and why — shares many parallels with the continued spread of the new coronavirus in the United States.
Unlike the situation in March, though, what’s happening in Europe isn’t necessarily a sign of what’s going to happen in the United States in the coming weeks or months, experts say.
In some ways, they note, what’s happening overseas has already happened and is still happening here.
They note there are still plenty of lessons to take from the current European COVID-19 spike, including how people react to restrictions, how to travel safely, and how to reopen (or not reopen) schools.
A uniquely European cause
In March and April, the COVID-19 experience of European countries such as Italy and the United Kingdom was seen as a preview of what was coming in the United States.
Those countries were widely seen as about 2 weeks ahead of where the United States would be in terms of new reported cases and deaths.
That’s likely not quite the case anymore, as the virus continued to spread through much of the United States over the summer while it was relatively contained in much of Europe.
Part of the reason, experts say, is because the current spike in Europe seems to be driven by a uniquely European factor: August holidays.
With new COVID-19 cases ebbing, many European nations started reopening their borders in mid-June. Travelers began to fly south for vacation like they would on any nonpandemic-ravaged year.
But outbreaks bloomed in summer holiday destinations, such as the French Riviera, Greece, and Croatia.
And then those travelers flew back to their home countries, where the outbreaks had been relatively contained.
In August, Italian officials said 30 percent of new cases were due to people who contracted the virus abroad. In Germany, officials put the figure at nearly 40 percent.
Americans, of course, go on vacation, too, but not all at once in August, and to a lot more destinations. There are a few parallels, however.
“We don’t have something like August vacation here, where lots of people converge on one spot, aside from something like spring break at Daytona Beach or somewhere… And we’ve already done that,” said Jeffrey Shaman, a professor of environmental health sciences at Columbia University in New York who has been leading modeling projects over the past several months to project how the virus is likely to spread in the United States.
Shaman told Healthline that what we’re seeing in Europe “is a function of their August vacations and going down to the Mediterranean and comingling and not using face masks. That’s what got the virus going again.”
There were numerous reports from destinations like the French Riviera about crowded parties with minimal use of face masks.
The situation echoes what was seen in some places in the United States during Memorial Day weekend, when crowded, maskless parties were tied to outbreaks.
That led to pleas for more caution — and even to closed beaches and parks — on the Fourth of July and, most recently, Labor Day weekend.
Whether new outbreaks spring up due to Labor Day get-togethers or Americans’ summer vacation trips remains to be seen. But seeing the European experience as a direct preview of what will happen here appears to no longer hold up.
People are people
There isn’t anything uniquely European about a crowd of people not wearing the recommended face masks or keeping their distance from each other, though.
“It has struck me that Europe is going through something of a process similar to ours, dividing itself into two populations: the careful and the careless,” Dr. William Schaffner, an infectious disease expert at Vanderbilt University in Tennessee, told Healthline.
The origins of these philosophies may be a bit different in Europe, he notes, but no matter the exact reasons, “there are people there who want to get out and congregate and not wear masks, like there are here, and the virus is looking for those people.”
Schaffner cites the experience in his home state of Tennessee, where the governor left mask rules up to the counties. Some of those mandates are now expiring.
That concerns him because of the scenes of so many young people out and about on past holidays and weekends, after which younger people became a greater proportion of positive cases and hospitalizations.
In Europe, younger people are also accounting for a growing percentage in the current surge.
Following the guidance can help solve that — on either continent. Schaffner says that after Nashville put a mask mandate in place and curtailed hours bars could be open, the numbers improved.
But no matter the continent, there are going to be people who refuse or struggle to follow that guidance.
“Human beings are human beings,” Schaffner said, “and there are a substantial number of people in the European countries that would like to be carefree and careless rather than continuing to be careful — and it’s the same in the U.S.”
Impact of schools reopening
On both continents, schools are also reopening.
One thing that’s stood out from Europe’s reopening of schools, though, is European officials’ apparent confidence that the reopening won’t necessarily exacerbate the virus’s spread.
“If the appropriate safety measures are applied, the probability of transmission is negligible,” Spain’s health emergency chief Fernando Simon said in late August.
Andrea Ammon, head of the European Centre for Disease Prevention and Control, told EU lawmakers on Sept. 2 that the reopening of schools doesn’t necessarily pose a higher risk if physical distancing and handwashing are implemented.
She cited evidence from the spring that reopening then hadn’t been tied to a spike in cases.
“I don’t agree with them,” Shaman said of European officials’ confidence. “The evidence continues to be mixed.”
He says that reopening in Denmark and Finland appeared to go OK, while Israel and South Korea had bigger issues.
“What’s been happening mostly is that people who want to reopen schools will point to evidence that children have been nominally involved in the transmission cycle, and those who do can point to evidence” that they do play a role, Shaman said. “The evidence is fairly clear that they lie somewhere in between.”
But the evidence you can’t find, he says, is that children play absolutely zero role: “Even if they’re not as efficient at spreading it, you’re creating opportunities for transmission.”
Hopefully, mitigation attempts via increased ventilation, limiting class sizes, face masks, and physical distancing have some effect, but it still depends on well you do it, Shaman says.
“Reopening schools is not going to benefit you in terms of the virus. It can only hurt there,” he said, though he noted there are many other benefits for both kids and parents.
“So, it’s not an easy issue regardless, but when I hear European leaders say it’s not going to be a problem, I’m just waiting for situations where they’re going to have flare-ups — I’m not saying they’re going to have lots, but there’s going to be some,” Shaman said.
Schaffner says the key thing is how much the virus is prevalent in the surrounding community.
In Europe, he said, “until recently, rates of COVID transmission in those communities was pretty low — that’s going to the be the single most important determinant in what happens here, in terms of how schools reopening affect the spread.”
By : Matt Berger
Date : September 13, 2020
Fact checked by : Michael Crescione
Source : Healthline
https://www.healthline.com/health-news/why-covid19-cases-in-europe-are-surging-back-to-march-levels
Southeast Asia: Six Tips for Unpacking COVID-19 Numbers
Seven months since the first COVID-19 case was reported in Southeast Asia and five months since lockdowns of various kinds and names became part of everyone’s lives, a good number of people are experiencing fatigue over figures, an overload of statistics, around the pandemic.
But COVID-19 has not been just a nasty typhoon that wreaks damage, then moves on. With no full treatment protocol or effective and safe vaccine, the pandemic persists even if many daily counts have now become weekly updates and statistics do not hog the headlines as they did months ago. Because COVID-19 is sticking around, the ability to process data around it is even more of a life skill amid at-times competing ‘conclusions’ about what they mean. It is certainly a lifesaving tool for individuals, as well news audiences, to make independent, informed decisions during these times.
Below are six tips for making our way through COVID-19 numbers:
1. Total cumulative cases of COVID-19 are often cited, but do not tell the whole story or allow for good comparison and too-quick conclusions about severity.
Is a country with more total cases worse off? Could be, but this first needs to be seen along other factors, as total confirmed cases are but one part of the story. Total confirmed cases acquire depth and fuller meaning against the backdrop of a country’s population size, speed and trend of growth (or changes) in cases over time, among others. A country may rank high in total cases, but have a less severe burden when its population size is factored in. This measurement of prevalence - proportion of cases in the population at a given time (100,000 people) - describes how widespread a disease is.
In ASEAN, Brunei has some 437,500 people and Indonesia has 274 million, so comparing gross COVID-19 figures does not work. Countries’ rankings may change when they are arranged by number of reported cases per 100,000 people. So while Singapore ranks third in Southeast Asia in total reported cases, it is first in terms of cases adjusted for population size (1,001 cases per 100,000 people on 25 August).
Even if a country starts to have fewer new cases daily, its cumulative figure will still go up since it adds from the first reported case onwards. The growth factor of cases would say more about the pandemic’s ‘pace’. “Case counts are only meaningful if we also know how much testing a country does,” according to the Our World in Data dashboard on COVID-19, which is run by Oxford University and Global Change Data Lab.
2. A more current description of the prevailing COVID-19 situation in a country lies in the number of still-active cases out of total cumulative cases.
‘Active’ means cases that are ongoing, unresolved, have not yet been reported or classified as recovered or died. Active cases don’t necessarily refer only to people in hospital (not all positive cases need confinement), and countries can have varying definitions. Active cases are those that remain in the pending folder, so to speak.
Lower proportions of active versus total cases are desirable, and a decline would show progress - a trend evident in countries with better recovery rates and lower mortality rates, such as Singapore and Thailand. Thailand has 3,401 confirmed cases, of which 108 or 3.17% are active (its count uses the phrase ‘receiving medical treatment’), as of 26 August.
Different country definitions of ‘active cases’ can affect COVID-19 counts - and a decline in active numbers usually goes with a rise in recoveries (assuming there is not a surge in fatalities). In some countries’ dashboards, a person who fares well is moved out of the active list to recoveries after a 30-day period. But in the Philippines, for instance, a person is defined as having recovered after a shorter period of 14 days’ quarantine (or when he or she tests negative). The moving by the Philippines, which has the most active COVID-19 cases in Southeast Asia, of huge cases numbers from the 'active' to the 'recovered' file led to very steep rises and plunges in its daily graphs. On a single day at end-July, it moved more than 37,000 active cases to the recovered list, and did the same for some 42,000 cases in one day in mid-August.
What does this tell us? It means that changes in classifications and definitions lead to adjustments that may look like progress, but are more mathematical shifts rather than a record of actual improvements on the ground.
3. We check mortality figures to gauge the likelihood of a person with COVID-19 dying from it, but there are limitations to what can be interpreted from these because the pandemic is still raging.
As in total cumulative cases, holding the number of total deaths up against other factors, including population size, provides a more contextualized picture.
The two usual datasets around fatalities are first, the current case-fatality ratio (CFR or number of deaths divided by reported absolute case numbers at a certain point) and second, fatalities per 100,000 people (general population, which comprises both confirmed cases and healthy people). The first set of figures shows the number of deaths against total confirmed cases at a point in time, and the second sets them in the context of population, which allows for comparison across countries.
Countries that score higher in these two yardsticks have the most deaths proportionally to their diagnosed COVID-19 cases or population sizes — but not necessarily the most number of deaths.
Take the Philippines and Indonesia, the two Southeast Asian nations hardest hit by COVID-19. As of 26 August, the Philippines’ CFR was 1.5%, lower than Indonesia’s 4.3%, but it had the highest deaths per 100,000 people in the region at 2.85, compared to Indonesia’s 2.56 (Indonesia accounts for 67% or so of the region’s deaths.) They are also the only Southeast Asian countries among the top 20 nations most affected by COVID-19, going by the Johns Hopkins University’s Coronavirus Resource Center. (Globally, the highest CFR is Mexico’s 10.8% and the most number of deaths per 100,000 population is Peru’s at 86.48, on 26 August.)
Respected sources such as the COVID-19 dashboards of Johns Hopkins University and Our World in Data, caution that CFR has limited use in defining risk. It does speak of disease severity but cannot be separated from its particular context, time and population. “During an outbreak of a pandemic, the CFR is a poor measure of the mortality risk,” explained the Our World in Data backgrounder on mortality.
As a pandemic rages, the numerator and denominator in the case-fatality formula - number of deaths and total confirmed cases - keep changing. Total case load is usually conclusive after a pandemic – a hundred deaths out of 10,000 cases paints a radically different picture from the same 100 deaths out of 100,000.
[‘Our World In Data’s section on mortality risk adds that crude mortality rate is different, and measures the probability that any person (not just infected ones) will die from a disease. It says the statistic we need - to answer the question ‘how likely is someone infected with COVID-19 to die’ - is the “infection fatality rate”, obtained from dividing number of deaths by final case numbers. An accurate figure for this is not yet possible as the number of total COVID-19 cases is not known, partly because not everyone with the virus is tested.
Amid the limitations of case-fatality rate, some groups have made efforts to compare a country’s deaths during a pandemic with its usual mortality rates, from all causes, in previous years. Computing for this “excess mortality”, which is the number of deaths above and beyond what is expected in non-pandemic situations, is an attempt to catch under-reporting of death figures, especially in settings with inadequate testing.
4. Testing is far from a simple story. It is crucial to the quality and context of other statistics, including a country’s total reported cases, which are in turn used to derive other figures.
RT-PCR (reverse transcription-polymerase chain reaction) testing needs to be done on an adequate scale, degree, with sound policy, against the size of a country’s outbreak, in order to be of most use in pandemic response. What is adequate, smart testing?
The World Health Organization (WHO) has suggested a positive rate lower than 10%, but better lower than 3%, as a benchmark of adequate testing. Countries that do very few tests per confirmed case are unlikely to be testing widely enough to find all cases. (See infographic called ‘How Many Tests Are Done Per New Case?’) Cases are likely going unreported if a country is testing too little versus its outbreak - that is, daily tests versus daily new confirmed cases per million people. Comparing testing to size of outbreak, beyond population size, is a major indicator. Having the most number of tests per million people is another matter from whether these tests are adequate for the scale of a country’s outbreak.
Could more tests account for more positive cases? It is one factor given that the deeper one digs, the more cases one may find. But the percentage of positives among total testing would be a telling and weighty factor.
In terms of testing rates versus population size, the Philippines has .29 tests per thousand (22 August), Indonesia .06 per thousand (25 August). These figures lag far behind those of the countries with the highest testing numbers of, say, 5 to 7.21 per thousand people.
By scale of outbreak, the higher and further to the right a country is in the chart on ‘Tests Vs the Scale of Outbreak’, the better it fares in the measure of daily tests per million people versus daily new confirmed cases per million people. Indonesia has 58 daily tests per million for an outbreak with 7.74 daily confirmed cases per million people, while the Philippines has 287 daily tests per million in an outbreak that sees 36.44 daily confirmed cases per million people. By number of people tested, Singapore has the highest rates at 1,088 daily tests per million people in its outbreak, which sees 12.14 new daily cases per million people.
5. To know better how transmissible the virus is, checking the positivity rate in COVID-19 tests and the basic reproduction number would be helpful in shaping the decisions people need to make during the pandemic.
The positive rate is the number of positive results from total tests, which can be reported as tests per day or cumulatively from the first COVID-19 case. It gives information about the virus’ spread, which is useful for making decisions around mobility. With adequate testing levels and scale, a decline in positivity is more welcome than the reverse, which suggests the virus is spreading faster. In countries with a high positive rate, the number of confirmed cases is likely to represent only a small fraction of the true number of infections, according to Our World in Data.
In terms of positivity rates from daily tests in Southeast Asia, the Philippines has the highest at 13% positivity and Indonesia 12.70%, as of 25 Aug, going by weekly rolling averages.
WHO defines a 5% positive rate or under as one indicator that a country is more able to control a pandemic. It advises that countries with daily positive rates of 5% or below, for at least two weeks, can more safely reopen economies – a level that Indonesia and the Philippines remain far from.
The reproduction number (‘R naught’) is an estimate of how many people are being infected by one person. The further up it is from 1 (one person infecting one other person), the more worrisome it is. An outbreak is considered under control if R naught stays at less than one. On 20 August, Jakarta Governor Anies Baswedan said the COVID-19[reproduction number in the Indonesian capital stood at 1.09. The Philippines’ reproduction number reached 1.61 in early August (it peaked at 2.62 in March), but eased to 1.1 and further to .963 on 23 August, according to data from the University of the Philippines COViD-19 dashboard] and experts from the same university.
6. The severity of COVID-19 is not defined by just a single statistic. If pandemic management were an orchestra, the various instruments in it need to make good harmony, that is, produce more effective responses.
The skill to evaluate key indicators can help individuals and communities make better decisions about their actions, and address their vulnerability in various settings. Caveats and context are part and parcel of statistics, and do not make them less important or valid. But it is easy to forget that when country and global dashboards use reported confirmed cases, they are in reality ‘the cases that we know of’ since tests were conducted on these people. In sum, ‘confirmed cases’ are not ’total actual cases’. Actual cases would number more than the confirmed cases being reported at present.
“In the COVID-19 pandemic we are in the unfortunate situation that the number of total cases is not known. Only a fraction of total cases - those confirmed by a test - is known,” the Our World in Data section on the global pandemic situation pointed out.
But progress is possible, as Our World in Data says, and some countries have managed better. Improvements show in several statistics, such as an easing in new cases and growth factors, more recoveries and fewer deaths, falling transmissibility of the virus.
“To end the coronavirus epidemic, we have a clear and simple goal: cases need to go to zero everywhere,” Our World in Data’s researchers said. “Only if we end the pandemic everywhere can the pandemic end anywhere.”
(Johanna Son is founder and editor of the 'Reporting ASEAN' series. Since March, she and colleague Yvonne T Chua, have been following the COVID-19 story in numbers in Southeast Asia. This article is part of Reporting ASEAN’s ‘Stories Behind the COVID-19 Series’, in partnership with Splice.)
By : Johanna Son
Date : August 29, 2020
Source : Vera Files https://verafiles.org/articles/southeast-asia-six-tips-unpacking-covid-19-numbers
COVID-19 and the End of Autocrats
The outbreak of COVID-19 initially looked like a gift to autocrats around the world — until they botched it.
The outbreak of COVID-19 initially looked like a gift to autocrats around the world. What better pretext for a state of emergency than a pandemic?
It was a golden opportunity to close borders, suppress civil society, and issue decrees left and right (mostly right). Donald Trump in the United States, Viktor Orbán in Hungary, Rodrigo Duterte in the Philippines, and others took advantage of the crisis to advance their me-first agendas and consolidate power. Best of all, they could count on the fear of infection to keep protestors off the streets.
However, as the global death toll approaches a million and autocrats face heightened criticism of their COVID responses, the pandemic is looking less and less like a gift.
The news from Mali, Belarus, and the Philippines should put the fear of regime change in the hearts of autocrats from Washington to Moscow. Despite all the recent signs that democracy is on the wane, people are voting with their feet by massing on the streets to make their voices heard, particularly in places where voting with their hands has not been honored.
The pandemic is not the only factor behind growing public disaffection for these strongmen. But for men whose chief selling point is strong leadership, the failure to contain a microscopic virus is pretty damning.
Yet, as the case of Belarus demonstrates, dictators do not give up power easily. And even when they do, as in Mali, it’s often military power, not people power, that fills the vacuum.
Meanwhile, all eyes are fixed on what will happen in the United States. Will American citizens take inspiration from the people of Belarus and Mali to remove their own elected autocrat?
People Power in Mali
Ibrahim Boubacar Keita (IBK) won the presidential election in Mali in 2013 in a landslide with 78 percent of the vote.
One of his chief selling points was a promise of “zero tolerance” for corruption. Easier said than done. The country was notoriously corrupt, and IBK had been in the thick of it during his tenure as prime minister in the 1990s. His return to power was also marked by corruption — a $40 million presidential jet, overpriced military imports, a son with expensive tastes — none of which goes over well in one of the poorest countries in the world.
Mali is not only poor, it’s conflict-prone. It has been subject to military coups at roughly 20-year intervals (1968, 1991, 2012). Several Islamist groups and a group of Tuareg separatists have battled the central government — and occasionally each other — over control of the country. French forces intervened at one point to suppress the Islamists, and France has been one of the strongest backers of IBK.
Mali held parliamentary elections in the spring, the first since 2013 after numerous delays. The turnout was low, due to coronavirus fears and sporadic violence as well as the sheer number of people displaced by conflict. Radical Islamists kidnapped the main opposition leader, Soumaila Cisse, three days before the first round. After the second round, IBK’s party, Rally for Mali, claimed a parliamentary majority, but only thanks to the Constitutional Court, which overturned the results for 31 seats and shifted the advantage to the ruling party.
This court decision sparked the initial protests. The main protest group, Movement of June 5 — Rally of Patriotic Force, eventually called for IBK’s resignation, the dissolution of parliament, and new elections. In July, government security forces tried to suppress the growing protests, killing more than a dozen people. International mediators were unable to resolve the stand-off. When IBK tried to pack the Constitutional Court with a new set of friends, protestors returned to the street.
On August 18, the military detained IBK and that night he stepped down. The coup was led by Assimi Goita, who’d worked closely with the U.S. military on counterinsurgency campaigns. Instead of acceding to demands for early elections, however, the new ruling junta says that Malians won’t go to the polls before 2023.
The people of Mali showed tremendous courage to stand up to their autocrat. Unfortunately, given the history of coups and various insurgencies, the military has gotten used to playing a dominant role in the country. The United States and France are also partly to blame for lavishing money, arms, and training on the army on behalf of their “war on terrorism” rather than rebuilding Mali’s economy and strengthening its political infrastructure.
Mali is a potent reminder that one alternative to autocrats is a military junta with little interest in democracy.
Democracy in Action in Belarus
Alexander Lukashenko is the longest serving leader in Europe. He’s been the president of Belarus since 1994, having risen to power like IBK on an anti-corruption platform. He’s never before faced much of a political challenge in the country’s tightly controlled elections.
Until these last elections.
In the August 9 elections, Lukashenko was seeking his sixth term in office. He expected smooth sailing since, after all, he’d jailed the country’s most prominent dissidents, he presided over loyal security forces, and he controlled the media.
But he didn’t control Svetlana Tikhanovskaya. The wife of jailed oppositionist Sergei Tikhanovsky managed to unite the opposition prior to the election and brought tens of thousands of people onto the streets for campaign rallies.
Nevertheless, Lukashenko declared victory in the election with 80 percent of the vote (even though he enjoyed, depending on which poll you consult, either a 33 percent or a 3 percent approval rating). Tikhanovskaya fled to Lithuania. And that seemed to be that.
Except that the citizens of Belarus are not accepting the results of the election.
As many as 200,000 people rallied in Minsk this Sunday to demand that Lukashenko step down. In U.S. terms, that would be as if 6 million Americans gathered in Washington to demand Trump’s resignation. So far, Lukashenko is ignoring the crowd’s demand. He has tried to send a signal of defiance by arriving at the presidential palace in a flak jacket and carrying an automatic weapon. More recently, he has resorted to quiet detentions and vague promises of reform.
Just like the Republicans who appeared as speakers at the Democratic convention, key people are abandoning Lukashenko’s side. The workers at the Minsk Tractor Factory are on an anti-Lukashenko strike, and many other workers at state-controlled enterprises have walked off the job. Police are quitting. The ambassador to Slovakia resigned. The state theaters have turned against the autocrat for the first time in 26 years.
Despite COVID-19, Belarus doesn’t have any prohibitions against mass gathering. That’s because Lukashenko has been a prominent COVID-19 denialist, refusing to shut down the country or adopt any significant medical precautions. His recommendations: take a sauna and drink vodka. Like Boris Johnson and Jair Bolsonaro, Lukashenko subsequently contracted the disease, though he claims that he was asymptomatic. The country has around 70,000 infections and about 650 deaths, but the numbers have started to rise again in recent days.
There are plenty of oppositionists ready to usher in democratic elections once Lukashenko is out of the way. A new coordinating council launched this month includes former culture minister Pavel Latushko as well as prominent dissidents like Olga Kovalkova and Maria Kolesnikova.
Even strong backing from Russia won’t help Lukashenko if the whole country turns against him. But beware the autocrat who can still count on support from a state apparatus and a militant minority.
The End of Duterte?
Nothing Rodrigo Duterte could do seemed to diminish his popularity in the Philippines. He insulted people left and right. He launched a war on drugs that left 27,000 alleged drug dealers dead from extrajudicial murders. Another 250 human rights defenders have also been killed.
Still, his approval ratings remained high, near 70 percent as recently as May.
But Duterte’s failure to deal with the coronavirus and the resulting economic dislocation may finally unseat him, if not from office then at least from the political imagination of Filipinos.
The Philippines now has around 200,000 infections and 3,000 deaths. Compared to the United States or Brazil, that might not sound like much. But surrounding the Philippines are countries that have dealt much more successfully with the pandemic: Thailand (58 deaths), Vietnam (27 deaths), Taiwan (7 deaths). Meanwhile, because of a strict lockdown that didn’t effectively contain the virus, the economy has crashed, and the country has entered its first recession in 29 years.
Like Trump, Duterte has blamed everyone but himself for the country’s failings, even unleashing a recent tirade against medical professionals. But Duterte’s insult politics is no longer working. As sociologist and former member of the Philippines parliament Walden Bello observes at Foreign Policy In Focus, “The hundreds of thousands blinded by his gangster charisma in the last 4 years have had the scales fall from their eyes and are now asking themselves how they could possibly have fallen in love with a person whose only skill was mass murder.”
In the Philippines, presidents serve one six-year term, and Duterte is four years into his. He may well attempt to hold on for two more years. He might even pull a Putin and change the constitution so that he can run again. A group of Duterte supporters recently held a press conference to call for a “revolutionary government” and a new constitution. Another possibility, in the wake of recent bombings in southern Philippines, might be a declaration of martial law to fight Abu Sayyaf, which is linked to the Islamic State.
But the combination of the pandemic, the economic crash, and a pro-China foreign policy may turn the population against Duterte so dramatically that he might view resignation as the only way out.
Democracy in the Balance
Plenty of autocrats still look pretty comfortable in their positions. Vladimir Putin — or forces loyal to him — just engineered the poisoning of one of his chief rivals, Alexei Navalny. Xi Jinping has just about turned Chinese politics into a one-man show. Viktor Orbán has consolidated his grip on power in Hungary, Recep Tayyip Erdo?an has suppressed or co-opted the opposition parties in Turkey, and Bashar al-Assad has seemingly weathered the civil war in Syria.
Even Brazilian President Jair Bolsonaro, despite an atrocious record on both the pandemic and the economy, has somehow managed to regain some popularity, with his approval rating nudging above his disapproval rating recently for the first time since April.
The U.S. presidential elections might tip the balance one way or the other. Although America still represents a democratic ideal for some around the world, that’s not the reason why the November elections matter. Donald Trump has so undermined democratic norms and institutions that democrats around the world are aghast that he hasn’t had to pay a political price. He escaped impeachment. His party still stands behind him. Plenty of his associates have gone to jail, but he has not (yet) been taken down by the courts.
That leaves the court of public opinion. If voters return Trump to office for a second term, it sends a strong signal that there are no penalties for ruining a democracy. Trump operates according to his own Pottery Barn rule: he broke a democracy and he believes that he now owns it. If voters agree, it will gladden the hearts of ruling autocrats and authoritarians-to-be all over the world.
Voting out Trump may not simply resuscitate American democracy. It may send a hopeful message to all those who oppose the Trump-like leaders in their lands.
Those leaders may have broken democracy, but we the people still own it.
By : John Feffer (John Feffer is the director of Foreign Policy In Focus.)
Date : August 26, 2020
Source : Foreign Policy in Focus https://fpif.org/covid-19-and-the-end-of-autocrats/
Did the COVID-19 pandemic revive nationalism?
It only took a sub-microscopic pathogen to confirm that, when a crisis strikes, it is the national framework that becomes crucial in offering a sense of security to disoriented masses.
If the present pandemic has shown anything, it is that nations matter. Yes, it seems quite obvious. But in a world traversed by incessant flows of information, goods, capital and, to a lesser extent, people, the fate of the nation has recurrently been depicted as doomed: an obsolescent socio-spatial register, out of tune with increasingly transnational and cosmopolitan societies. And yet, it only took a sub-microscopic pathogen to confirm that, when a crisis strikes, it is the national framework that becomes crucial in offering a sense of security to disoriented masses.
In what follows, I would like to use the case of Italy (the country of my nationality) and the United Kingdom (my country of residence) to reflect on what we can learn about the nation facing the present global pandemic. I am not interested here in governmental responses which have securitised the health threat in terms of a threat to national security (despite the virus being a global threat). Neither am I interested in the militaristic language deployed by many national governments and mass media to respond to this threat, which equally reinforces national borders as the principal lines of defence against the virus. My interest instead is in the emotional responses of the general public facing the pandemic and the extent to which these responses have contributed to reproduce a sense of nationhood.
When Italy became the first European country to experience the highest levels of coronavirus contagion and related deaths, my cousin forwarded me a video which was circulating on social media. Produced and aired by a popular Italian radio (Radio 105), the video narrates the stories of ordinary and famous Italians who directed their courage and inventiveness towards helping the nation fight the virus. The message of the video, like others which can be found on the web, is imbued with feelings of national pride and solidarity.
What’s more, after showcasing the Italian spirit of abnegation, the video ends with the phrase: “but the others cannot understand all this because… they are not Italians”. Italy is unique. Italians have no match in the world. A sense of national exceptionalism, merged with feelings of pride and solidarity, heralds the nation as the main register of identification in times of crisis. Singing from balconies and flagging rainbow drawings with the phrase “andrà tutto bene” (everything will be all right) have also become spontaneous widespread practices, helping people to find a sense of security, reassurance and hope within this shared national atmosphere.
The UK has not been different. From the beginning of the pandemic, the government’s slogan ‘Stay Home, Protect the NHS, Save Lives’ has deeply resonated with people’s feelings. In the British national narrative, the NHS is a national symbol, highly valued by the British people who, in a survey, listed it at the top of the things that make them proud to be British. Thus, it was no surprise to see the success of the grassroot initiative ‘Clap for our Carers’, which every Thursday at 8pm saw millions of people clapping and banging pots and pans to pay respect to the NHS and other key workers.
The same enthusiasm moved a World War II veteran, Captain Tom, to walk 100 laps around his garden to raise money for the NHS. His challenge ‘captured the hearts’ of the whole nation, no less than the millions of rainbows drawn by children to symbolise national resilience and hope. Here, like in Italy, an atmosphere of national affect brought people together, confirming how the nation is something to celebrate, identify with and hold on to in times of uncertainty.
But it would be erroneous to think that the coronavirus has simply reinforced the thrust of the nation in an increasingly – at least until recently – globalising world. The same pandemic has in fact revealed, both in Italy and in the UK, how the nation is far from such a unified and unifying register.
In Britain, for instance, many of the heroes acclaimed every Thursday evening have turned out to be denizens, often racialized minorities, who, according to the new point-based immigration system, might have no place in a post-Brexit Britain. The higher coronavirus death rate among ethnic minorities has also exposed the persistent socio-economic divides which run deeply within the British nation.
In the case of Italy, ethnic minorities have been completely absent from any media coverage of the pandemic, offering the flawed perception that Italy continues to remain an ethnically homogeneous nation when in fact about 10% of its population is foreign born.
The pandemic has also exposed deep-seated territorial fractures. Scotland, Wales and Northern Ireland have adopted different measures to contain the virus compared to England: different policies which also speak of profound national differences. Similarly, in Italy, regional powers have adopted different measures to deal with the spread of the virus, putting the regional interest before the national one, particularly when it came to end the lockdown.
If the pandemic shows that nations matter, particularly as affective spaces in times of crisis, it also shows that nations continue to remain contested spaces, riddled with social tensions and territorial fractures. In other words, the pandemic has not exposed something which we did not know about the nation, but simply amplified, on the one hand, affective manifestations which concur to reproduce the nation in the everyday life and, on the other hand, lines of ethno-racial and territorial divisions which persist beyond the fleeting moment of singing or clapping together.
If, during the pandemic, governments have capitalised on popular manifestations of affective nationalism, which have helped them side-line the above mentioned tensions and fractures, it is likely that in the aftermath of the pandemic these tensions and fractures will appear with new vigour, fuelled by the economic havoc produced by the pandemic. The unifying power of affective nationalism will be tested then.
By : Marco Antonsich
Date : July 22, 2020
Source : Open Democracy
https://www.opendemocracy.net/en/pandemic-border/did-covid-19-pandemic-revive-nationalism/
Getting to grips with the COVID-19 outbreak in Nigeria
The pace of SARS-CoV-2 transmission has triggered different government responses globally. These have had varying levels of effectiveness and some unintended outcomes.
Nigeria, Africa’s most populous country with many densely populated cities, presents a unique situation for the explosive spread of SARS-CoV-2. Factors include high population density, limited health-care resources and access, and a high poverty index among a range of other socioeconomic factors.
Yet, by early August the number of reported confirmed infections (44,443) and mortality (910) was lower than other countries with dense urban populations and similar socioeconomic challenges.
As we point out in our paper, Insights into the Nigerian CoVID-19 Outbreak, the exact reasons for this are not clear but might include societal, immunological, epidemiological, political and infrastructural factors.
In our paper we set out to describe the ongoing CoVID-19 outbreak and its associated peculiarities. We also identify critical steps that still need to be taken to contain and control the outbreak.
Insights
We found that the CoVID-19 outbreak in Nigeria showed age and sex specific differences. More young people were affected compared to older people. This was different to the global trend.
This age-specific difference was also seen across other African countries. Examples include Ghana and South Africa.
We hypothesise that the age difference in the profile of cases in Nigeria could be due to the lower median age (a more youthful population) in Nigeria and Africa compared to the US and European countries.
Also, there was a sex and gender-based difference in the severity of the outbreak in Nigeria. More males than females have been infected. This is similar to patterns elsewhere in the world.
The reason for this is not clear. Several factors have been suggested. These include the role of sex hormones in the regulation of immune response and the expression of the SARS-CoV-2 receptor.
The expression of the viral receptor - ACE2 - in the Nigerian population should be investigated using various tools such as immunogenetics. This kind of study would help us understand differences in the expression of the receptor across the country, and how this has affected the outcome of the disease.
In immunology, constant exposure to disease causing agents (pathogens) like viruses makes a critical arm of the immune system (innate immune system) more primed to be able to respond quicker and faster to different pathogens. This concept – called trained immunity – is being debated as a possible explanation for the low COVID-19 incidence in Nigeria and Africa due to constant exposure and high burden of different infectious disease.
However, the benefits or detriments of this still have to be fully explored.
Lastly, we argue that public mistrust, misinformation and disinformation could be a major driver of COVID-19 in Nigeria. This mistrust has been an offshoot of the initial widespread dismissal of the reported cases as a “disease of the elite” and an embezzlement ploy for allocated response funds.
This was further reinforced by conspiracy theories emanating from various traditional and online media sources. The consequences of this mistrust were reflected in non-compliance with lockdown rules and social distancing restrictions. This potentially undermined the impact of the government containment response.
Modelling
Our research used the age-stratified SEIR (susceptible-exposed-infected-recovered) model to predict and model the Nigerian COVID-19 outbreak.
This showed that Nigeria is still in the early stages of the outbreak. The expected trajectory depends on the mitigation measures to contain the spread. A surge is expected in the coming months.
It is important to note that the COVID-19 situation in Nigeria is fast evolving. It is therefore difficult to ascertain the efficacy of the mitigation measures.
In addition, this is only a prediction and comes with a level of uncertainty in the parameters and the simplification of the model we used. As with all models, it might not capture the full complexity of the outbreak. But it can help better understand the dynamics of the outbreak. And it can inform government decisions on future interventions.
Consequence and impact
The incidence and spread of COVID-19 has affected Nigerian public health facilities both negatively and positively.
One of the negative consequences includes the impact on other infectious diseases. For example, an evaluation of the Lassa fever epidemiological trend over the past 5 years (2016 – 2020) of the same reporting period (week 1 – 23) also indicates the highest case peak reported in 2020.
This surge might not be absolutely associated with the current COVID-19 outbreak. But the impact of the outbreak would undoubtedly influence resource allocation and the working capacity of the national public health infrastructure.
This suggests that the current pandemic could affect the epidemiology and response to other endemic and integrated diseases. These include cerebrospinal meningitis, malaria, cholera, measles, Lassa fever and Yellow fever.
On a positive note, the COVID-19 outbreak has brought improvements to the health sector. This has included an increase in the implementation of the collaborative One-Health approach. This involves the collaborative participation of stakeholders from the human, animal and environmental health sector.
Examples include the incorporation of veterinarians and environmentalists in the Joint Task Force in response to CoVID-19, and port authorities in the establishment of the Coronavirus preparedness group.
There has also been rapid scale-up and activation of various stand alone laboratories. Lastly, the pandemic has highlighted the enormous potential for genomic surveillance in Nigeria.
But the COVID-19 outbreak, like other infectious disease outbreaks, has exposed the fragile health system in Nigeria. The lack of adequate testing, the poor health infrastructure, sub-optimal investment and funding in the STEM field and inadequate trained health professionals, leave Nigeria on an unknown trajectory.
As we work towards returning to normal, we argue that Nigeria’s leeway out of the COVID-19 outbreak, and other future outbreaks, will require improved diagnostic capacity, effective testing and tracing, and massive investment in research and health infrastructures.
By : Oyebola Oyesola (Recent PhD graduate from Cornell University, Cornell University)
Christian Happi (Professor of Molecular Biology and Genomics, Redeemer's University)
Christian Happi (Professor of Molecular Biology and Genomics, Redeemer's University)
Dr Chinedu Ugwu A (Research Fellow/Lecturer, Africa Centre of Excellence for Genomics of
Infectious Disease (ACEGID), Redeemer's University, Redeemer's University)
Jonathan Heeney (Professor of Comparative Pathology, Cambridge University,
University of Cambridge)
Opeoluwa Adewale-Fasoro (Researcher, Molecular Microbiology and Immunology department,
Johns Hopkins Bloomberg School of Public Health, Johns Hopkins Bloomberg School of Public Health)
Date : August 11, 2020
Source : The Conversation
https://theconversation.com/getting-to-grips-with-the-covid-19-outbreak-in-nigeria-143943
A potential new weapon in the fight against COVID-19: Food coloring
The big idea
Our biomedical engineering lab has developed a way to potentially neutralize viruses lingering in the air using aerosols of FDA-approved food coloring dyes. Aerosols are tiny bits of solid or liquid matter suspended in air.
Our idea was inspired by photodynamic therapy, which is a medical treatment, including for certain types of cancer. Photodynamic therapy uses a photosensitizer, a chemical that reacts with oxygen in the presence of light, to produce oxygen free radicals. These radicals are highly reactive, meaning they trigger other chemical reactions, including ones that kill harmful pathogens.
Instead of using expensive medical photosensitizers, we have identified several FDA-approved food coloring dyes that can be used to generate free radicals in visible light. We use ultrasound to generate small aerosols containing the food coloring so that the dyes can float and linger in the air. The aerosols are barely visible, and their small size and short lifespan in light means they don’t stain surfaces.
We used this technique to produce a device, Photodynamic Airborne Cleaner, that disinfects pathogens floating in the air. To the best of our knowledge, this is the first-of-its-kind photodynamic therapy aerosol generator for airborne disinfection.
Why it matters
Viruses and bacteria are often transmitted through the air. A person infected with SARS-CoV-2, the virus that causes COVID-19, who coughs or sneezes produces virus-containing droplets and aerosols that float in the air and can cause infection.
Due to this risk, all kinds of indoor gatherings are now limited. It is critical to be able to disinfect and sanitize large volumes of indoor air where many people are present to reduce the chances of transmission.
What other research is being done in this field
Photodynamic therapy was first demonstrated as a means of fighting bacterial infection. Oxygen free radicals, specifically singlet oxygen, can also inactivate viruses by damaging the nucleic acids, proteins and lipids that they are composed of. In particular, singlet oxygen is effective at breaking down the lipid envelopes that form protective shells around many viruses. Most of the viruses that are harmful to humans, including SARS-CoV-2, have these envelopes.
Several other disinfection techniques are available, for example aerosolized hydrogen peroxide, hydrogen peroxide vapor, ozone, steam and UV-C or “deep UV” illumination. However, these are more appropriate for disinfecting surfaces than disabling pathogens floating in the air. Also, they can be hazardous to humans. For example, deep UV is commonly used as a disinfectant, but is carcinogenic.
What’s next
We are preparing to collaborate with a federal research team to evaluate the effectiveness of our Photodynamic Airborne Cleaner against airborne transmission of SARS-CoV-2.
Aerosols of FDA-approved food coloring dyes and their singlet oxygen generation do not last for a long time. These dye aerosols break down in light, and singlet oxygen is not generated without light. Nevertheless, even though the food coloring is FDA-approved for consumption, it’s necessary to test the safety of potential inhalation and oral intake.
By :
Young Kim (Associate Professor of Biomedical Engineering, Purdue University)
Hee-Jae Jeon (Postdoctoral Fellow, Biomedical Engineering, Purdue University)
Jung Woo Leem (Postdoctoral Fellow, Biomedical Engineering, Purdue University)
Yuhyun Ji (Doctoral student in Biomedical Engineering, Purdue University)
Date : August 20, 2020
Source : The Conversation
https://theconversation.com/a-potential-new-weapon-in-the-fight-against-covid-19-food-coloring-144177
Might social intelligence save Latin America from its governments in times of Covid-19?
Digital democratic innovation as a response to Covid-19 puts on the table the need for governments to rely on society to advance solutions to new and complex problems.
The Covid-19 pandemic triggered a multitude of various unforeseen problems, and most governments around the world were unprepared, finding themselves urged to design responses in a very short period of time and under highly uncertain conditions. In countries with low state capacity and high social inequality, the challenges have been even greater.
Government responses have been limited by lack of resources, infrastructure, and knowledge, in addition to the burden of having to immediately handle long-standing social fissures that quickly revealed that not all are equal before the virus.
In Latin America, where state capacity is characteristically low and inequality high, the coronavirus found optimal conditions for proliferation. In some countries, the sanitary emergency has also been aggravated by the economic crisis, social unrest, and political instability. Five out of the ten countries hit hardest by the pandemic so far are located in Latin America, and about one-third of all global deaths due to the virus have occurred in the region.
No response could have been rapid enough to address centuries-long problems such as political exclusion and social inequality, or effective enough to circumvent the deep-rooted lack of accountability engrained in political institutions. But had actual political leadership not been absent and had governments taken proper action – which was definitely not the case in several countries – much could have been done to prevent the pandemic from swiftly becoming pandemonium.
The Covid-19 pandemic presents an opportunity to test the potential of social intelligence as fuel for processes of creative collaboration that may aid governments to reinvent themselves.
In such scenarios, it seems relevant to acknowledge the limits of the state to deal with huge and unpredictable challenges and thus the need to resort to civil society. State capacity cannot be built overnight, but social intelligence is an unlimited and permanently available resource. In recent years, digital technology has multiplied what has been long called social intelligence (Dewey) and is now more often known as collective intelligence (Lévy), the wisdom of crowds (Surowiecki), or democratic reason (Landemore).
Taken together, these concepts point to the most powerful tool available to governments facing hard problems and unprecedented challenges: the sourcing and sharing of knowledge, information, skills, resources, and data from citizens in order to address social and political problems.
The Covid-19 pandemic presents an opportunity to test the potential of social intelligence as fuel for processes of creative collaboration that may aid governments to reinvent themselves and prepare for the challenges that will remain after the virus is gone. By creative collaboration, I mean a range of forms of communication, action, and connection among citizens themselves, between citizens and civil society organizations (CSOs), and between the latter two and their governments, all with the common aim of addressing problems that affect all and that the state for various reasons cannot (satisfactorily) respond to alone.
While several Latin American countries have been stuck in the Covid-19 crisis with governments unable or unwilling to contain it or to reduce its damages, a substantial number of digital democratic innovations have been advanced by civil society in the past few months. These comprise institutions, processes, and mechanisms that rely on digital citizen participation as a means to address social and political problems – and, more recently, also problems of a humanitarian nature.
Crowdsourcing
The problem-solving nature of democratic innovations consists of identifying needs and issues that require a political decision or action, in addition to enabling citizens to take part in the formulation, implementation, and evaluation of such decisions and actions. Digital technologies allow democratic innovations to operate as catalyzers of social intelligence, turning citizens into problem solvers as they contribute knowledge, information, data, and skills to address common problems that should in fact be handled by governments.
What is generally called crowdsourcing comprises the most successful combination of social intelligence and digital technology known to date. By amassing knowledge from citizens, governments can gather sizeable amounts of information from sources that would otherwise probably not be accessible. Crowdsourcing mostly facilitates the gathering of ideas, expertise, and data. It allows an unlimited number of citizens to participate in and contribute to all stages of the policy cycle.
Mechanisms for knowledge-gathering are effective tools to identify problems, assess their possible solutions, and collect inputs necessary for the successful implementation of the latter. Crowdsourcing thus enables the use of social intelligence to solve political and social problems and improve government policies and actions, especially when the state is overwhelmed, as happens in contexts of emergency and times of uncertainty.
Digital democratic innovations
Between March 16 and July 1 of this year, at least 400 digital democratic innovations were created across 18 countries in Latin America with the specific aim of handling the Covid-19 crisis and mitigating its impact, according to recent data from the LATINNO project. These innovations are essentially mechanisms and processes in which citizens, with the aid of digital tools, are enabled to address social, political, and humanitarian problems related to the pandemic.
Citizens engage in and contribute to three levels of responses, which are based on information, connection, and action. About one-fourth of these digital democratic innovations clearly rely on crowdsourcing social intelligence.
The great majority of those digital innovations have been developed by CSOs. Around 75% of them have no government involvement at all, which is striking in a region known for implementing state-driven citizen participation as a result of the democratization processes that took place in the late 20th century. Civil society has stepped in in most countries, particularly where government responses were absent (Brazil and Nicaragua), slow (Mexico), insufficient due to lack of economic resources (Argentina) or infrastructure (Peru), or simply inefficient (Chile).
When the state acts in concert with civil society, and resorts to it in order to address concrete problems, democracy is the main winner.
Based on these data from 18 Latin American countries, one can observe that digital democratic innovations address challenges posed by the Covid-19 outbreak in five main ways: first, generating verified information and reliable data; second, geolocating problems, needs, and demands; third, mobilizing resources, skills, and knowledge to address those problems, needs, and demands; fourth, connecting demand (individuals and organizations in need) and supply (individuals and organizations willing to provide whatever is needed); and fifth and finally, implementing and monitoring public policies and actions. In some countries, there is a sixth use that cuts across the other five: assisting vulnerable groups such as the elderly, women, children and youth, indigenous peoples, and Afro-descendants.
The five main uses of digital democratic innovations designed to handle problems resulting from the pandemic become clearer as one observes how social intelligence, with the aid of digital tools, operates in four dimensions, or moments, each of which concerned with the following activities:
Identification of Problems:
- Identification and geolocation of needs, shortages, deficiencies, and demands
- Identification of limitations in public service delivery and institutional performance
- Identification of groups, communities, and neighborhoods with greater or special needs
Generation of Knowledge:
- Production, collection, and aggregation of data from citizens
- Crowdsourcing of knowledge, information, ideas, resources, assets, and skills
- Fact and data checking and dissemination of verified information
Design of Solutions:
- Collaborative design of alternative solutions from and within civil society
- Integration of citizen and CSO contributions to government responses
Implementation of Responses:
- Collaborative implementation of responses
- Direct involvement of citizens in service provision or supply generation
Although empirically observed during the Covid-19 crisis in Latin America, these four dimensions, or moments, of social intelligence are expandable to any situation in which citizens and CSOs step in to make up for state deficiencies, handling challenges that cannot be properly and satisfactorily resolved by their governments alone. When applied to the sanitary crisis, the activities listed above are translated into quite specific goals that aim at addressing different problems related to the spread of the virus in the region, as summarized and exemplified in the table below.
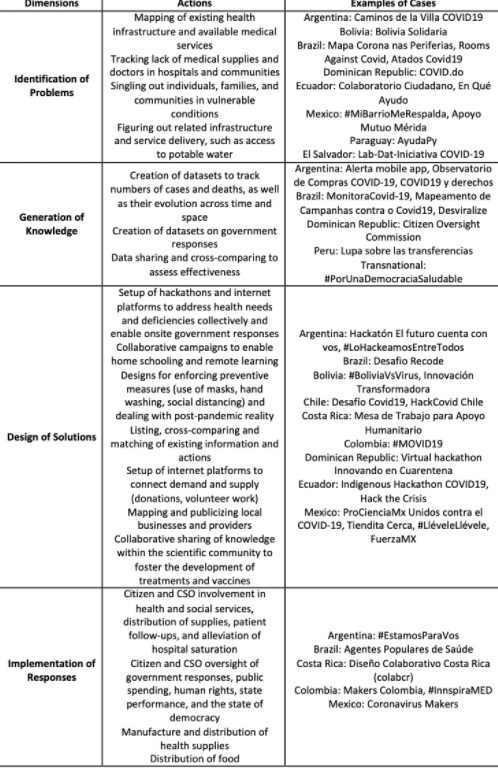
In its pragmatist origin, the concept of intelligence is closely related to those of action and creativity. Social intelligence is composed of creative actions of citizens and their organizations. When the state acts in concert with civil society, and resorts to it in order to address concrete problems, democracy is the main winner.
In a democracy, to exercise power is to “act in concert” (Arendt). The Covid-19 crisis has been showing that some social and political challenges can only be dealt with if one acts in concert with others and that democracy can only recover from the virus if the cure involves citizens, civil society, and governments alike.
By : Thamy Pogrebinschi
Date : August 18, 2020
Source : Open Democracy
https://www.opendemocracy.net/en/democraciaabierta/puede-la-inteligencia-social-salvar-a-america-latina-de-sus-gobiernos-en-tiempos-de-covid-en/
Laying bare the social and economic fault lines: India’s COVID-19 experience
Women in India spend 297 minutes on unpaid domestic work each day, 245 minutes more than men who contribute only 52 minutes. Women’s work is not accounted for in the national accounting system, making their contributions unrecognised and unvalued.
An Oxfam report observes that the unpaid work of Indian women plays a crucial role in sustaining economic activity, equivalent to 3.1 per cent of GDP. Economic and social challenges, including domestic violence, dowry at the time of marriage and the trafficking of women, coalesce to sustain and perpetuate gender inequalities in India.
COVID-19 and the ensuing lockdowns worldwide have forced markets and the movement of people to a standstill. But the unpaid care economy has continued to function unabated. According to the International Labour Organization, globally women perform 76.2 per cent of all unpaid care work. The economic contribution is estimated to be US$10 trillion a year and 13 per cent of global GDP.
COVID-19 has seen the ‘domestic’ space reclaimed as one that can accommodate economic work. Individuals in IT-enabled services have for more than two decades blurred the ‘public’ and the ‘private’, and the ‘office’ and the ‘home’, through telecommuting. The closure of establishments like schools, creche facilities, laundromats and cleaning services, and the restriction on the entry of care and household workers due to the need for social distancing, has brought many monetised domestic tasks back to the confines of the domestic. For the first time in the post-war era, society is witnessing the blurring of this divide on a large scale.
The division of the ‘production’ and ‘reproduction’ spheres occurred in the Industrial Revolution. The work done in the ‘reproduction’ sphere — procreation, care work and socialisation of young children — has been labelled emotional labour. Feminist Maria Mies called this ‘production of life’ or ‘subsistence work’, constituting the hidden underground world of capitalism and accumulation. The COVID-19-induced collapsing of this division between ‘production’ and ‘reproduction’ has put a spotlight on the political economy of their compartmentalisation, hierarchisation and invisibilisation from discourse and public policy.
Women’s labour, understood as a ‘reserve army of labour’, contracts or expands with the demand for labour in the market. Their contribution to procreation — replacing labour through fertility — is unpaid, unrecognised and inadequately supported by markets or state policies. Domestic labour helps capitalism in keeping the ‘real wages’ of workers low on the one hand while keeping the demand for goods and services ticking on the other. Ivan Illich refers to domestic work as ‘shadow work’ and traces its emergence to the rise of industrialisation.
Apart from expanded workdays within the domestic sphere, another aspect that has become hyper-visible during the COVID-19 lockdown is the plight of India’s internal migrants who form part of the unorganised and informal sectors of the economy. Migrants with few rights or entitlements constitute the other ‘reserve army’ of labour. The announcement of the lockdown on 24 March 2020, with four hours’ notice, clearly signalled that the Indian government did not foresee the fallout of such an announcement on precarious workers, who seem to be perceived as dispensable to the urban economy.
In the post-liberalisation period in India, growth in regular and secure employment has given way to informality and precarity. Only 23 per cent of the workforce is regularly employed, 52 per cent are self-employed and 25 per cent are casually employed. According to the 2017–18 Periodic Labour Force Survey, the informal sector makes up about 65 per cent of India’s workforce. 88 per cent of women’s employment in India is in the informal sector while 30 per cent of the total population migrates internally.
The economic recession following COVID-19 is lifting the lid off the globalisation ‘success’ story of India and many other countries wedded to the current market model. Women as workers, farmers, artisans, self-employed, unpaid family workers, mothers, caregivers and nurturers are left to carry on with their domestic and caregiving tasks in the absence of any wider support for these services. The unprecedented exodus of internal migrant workers to their home states has driven home the point that their rights as citizens and workers have been short-changed.
Post-COVID-19, can India aspire to be a society where work is recognised, legislated and supported whether it is done at home or in the public domain, and whether it is done for the market or subsistence? The distress that women and informal sector workers are enduring can be vindicated if binaries in society and economy can be blurred towards a more humane world that is not dominated by corporate interests and global politics.
Lakshmi Lingam is Professor and Dean at the School of Media and Cultural Studies, Tata Institute of Social Studies, Mumbai.
This article is part of an EAF special feature series on the novel coronavirus crisis and its impact.
By : Lakshmi Lingam, Tata Institute of Social Sciences
Date : August 15, 2020
Source : East Asia Forum
https://www.eastasiaforum.org/2020/08/15/laying-bare-the-social-and-economic-fault-lines-indias-covid-19-experience/
2 in 5 schools around the world lacked basic handwashing facilities prior to COVID-19 pandemic — UNICEF, WHO
As schools worldwide struggle with reopening, the latest data from the WHO/UNICEF Joint Monitoring Programme (JMP) reveal that 43 per cent of schools around the world lacked access to basic handwashing with soap and water in 2019 – a key condition for schools to be able to operate safely in the midst of the COVID-19 pandemic.
“Global school closures since the onset of the COVID-19 pandemic have presented an unprecedented challenge to children’s education and wellbeing,” said Henrietta Fore, UNICEF Executive Director. “We must prioritize children’s learning. This means making sure that schools are safe to reopen – including with access to hand hygiene, clean drinking water and safe sanitation.”
According to the report, around 818 million children lack basic handwashing facilities at their schools, which puts them at increased risk of COVID-19 and other transmittable diseases. More than one third of these children (295 million) are from sub-Saharan Africa. In the least developed countries, 7 out of 10 schools lack basic handwashing facilities and half of schools lack basic sanitation and water services.
The report stresses that governments seeking to control the spread of COVID-19 must balance the need for implementation of public health measures versus the associated social and economic impacts of lockdown measures. Evidence of the negative impacts of prolonged school closures on children’s safety, wellbeing and learning are well-documented, the report says.
“Access to water, sanitation and hygiene services is essential for effective infection prevention and control in all settings, including schools," said Dr Tedros Adhanom Ghebreyesus, WHO Director-General. "It must be a major focus of government strategies for the safe reopening and operation of schools during the ongoing COVID-19 global pandemic.”
Other key findings from the report include:
Of the 818 million children who lacked a basic handwashing service at their school, 355 million went to schools which had facilities with water but no soap, and 462 million to schools which had no facilities or water available for handwashing.
In the 60 countries at highest risk of health and humanitarian crises due to COVID-19, 3 in 4 children lacked basic handwashing service at their school at the start of the outbreak; half of all children lacked basic water service; and more than half lacked basic sanitation service.
1 in 3 schools worldwide had either limited drinking water service or no drinking water service at all.
698 million children lacked basic sanitation service at their school.
The report identifies several resources necessary for COVID-19 prevention and control in schools, including 10 immediate actions and safety checklists. It builds on guidelines on the safe reopening of schools issued by UNESCO, UNICEF, WFP and the World Bank with practical advice for national and local authorities on how to prepare for safe school reopening and keep children safe when they return to school. The guidelines include several WASH-related protocols on hygiene measures, use of personal protective equipment, cleaning and disinfection, as well as providing access to clean water, handwashing stations with soap, and safe toilets.
UNICEF and WHO are committed to achieving equitable access to adequate WASH services worldwide. The agencies recently launched a joint initiative, Hand Hygiene for All, to support the most vulnerable communities with the means to protect their health and environment. It brings together international partners, national governments, public and private sectors, and civil society to ensure affordable products and services are available, especially in disadvantaged areas.
###
For further information, please contact:
Sara Alhattab, UNICEF Headquarters (working out of Jordan), Tel: +962 7 80180363, [email protected]
WHO Media Enquiries: Tel: +41 22 791 2222, [email protected]
About UNICEF
UNICEF works in some of the world’s toughest places, to reach the world’s most disadvantaged children. Across more than 190 countries and territories, we work for every child, everywhere, to build a better world for everyone.
Follow UNICEF on Twitter and Facebook
About WHO
The World Health Organization directs and coordinates international health within the United Nations system. Working with its 194 Member States, WHO’s mission is to promote health, keep the world safe and serve the vulnerable.
For more information about WHO, visit www.who.int.
Follow WHO on Twitter and Facebook
About the Joint Monitoring Programme
The WHO/UNICEF Joint Monitoring Programme (JMP) for Water Supply, Sanitation and Hygiene is responsible for monitoring global progress towards the Sustainable Development Goal (SDG) targets and indicators relating drinking water, sanitation and hygiene (WASH). The JMP produces national, regional and global estimates of progress on WASH in households, schools and health care facilities.
COVID-19 in Southeast Asia: non-citizens have a right to protection too
Arbitrary differentiation between citizen and non-citizen is causing migrants to suffer the worst of the pandemic.
Singapore leads the region in COVID-19 with 28,794 confirmed cases as of 19 May 2020. The majority of Singapore’s cases come from crowded foreign-worker dormitories. Singapore is just one of a number of countries in the region where millions of migrant workers concentrate. The accurate number of migrants is difficult to gauge but it’s estimated that in 2019, around 7-8 million migrants are working in Brunei Darussalam (40% of the total population), Malaysia (2-3 million), Singapore (around 1.3 million), and Thailand (3-4 million). These population are at high risk of infection.
This pandemic has brought up issues of ‘hidden apartheid’ not only on grounds of race but also of citizenship. While Covid 19 can infect anyone, some groups are disproportionately affected especially migrants. Border closing and the delineation between ‘citizens’ and ‘non citizens’ is not only contributing to the public health crisis but is also having a devastating effect on the rights and plight of migrant workers.
The practice of excluding non-citizens from essential health services presents a paradox. The paradox of controlling them in confined spaces while advising populations to respect social distancing; paradox of caring for citizens while limiting resources to care for non-citizens who contribute, as much as citizens, to the economy of a country. In Singapore, this paradox has already resulted in a high price that the state has to pay.
For the past two decades, I have been engaging intensively with issues of migration especially in Southeast Asia. As a researcher of migration and an advocate for the rights of migrants in Southeast Asia, I feel obligated to share my views which, I hope, will generate some reflections and change, even if only a small one, on the treatment of non-citizens.
The daily images of migrant workers living in cramped and dilapidated dormitories/housing facilities with poor hygienic conditions in Malaysia, Singapore and Thailand raise serious concerns about a possible uncontrollable outbreak of COVID-19 among migrants. In Singapore, before the discovery of a high number of cases of COVID-19 among migrant workers, government distribution of face masks and hand sanitizer was limited only to citizens. Non-citizens and migrant workers were not entitled to such courtesy. In Thailand, migrant workers, especially those in informal sectors such as domestic work, agriculture, are not eligible for unemployment benefits. In Malaysia, even though the authorities announced free COVID-19 screening and testing for foreigners including migrant workers, refugees and asylum seekers, it was not clear whether those who test positive would have to pay “foreigner fee” for treatment; and the risk is even higher for stateless persons in the country.
Many migrants, documented or undocumented, and stateless persons, lost their means of living because of the shutdown in all countries in Southeast Asia and have been excluded from the preventive health and treatment mechanisms.
The citizen and non-citizen divide shaped by the concept of nation state and deployed to secure the dominance of ‘citizens’, inevitably marginalizes particular groups considered ‘different’. This practice of ‘differencing’ is reflected in the allocation of resources to citizens who are members of a political community. Non-citizens are not usually entitled to the same ‘membership goods’ such as employment, emergency services and economic resources, political participation, immunity from expulsion and a legal status.
In the context of COVID-19, this refers to health services, access to proper information, right to freedom of movement and expression, right to adequate housing and right to social security/compensation and any other humanitarian assistance that any person should enjoy. The access to ‘membership goods’ depends very much on laws and policies of a particular country, on political will and level of openness of both state and society.
Such arbitrary differentiation between citizen and non-citizen causes migrants to suffer the worst of pandemic. Such a differentiation during a global health crisis which does not spare any person is a reflection of a ‘value based exclusion’ which serves to hide a much deeper form of injustice and inequality within society. In so doing, states will equally suffer the worst health scenario as already seen in some countries such as Singapore. States are urged to apply a more inclusive social protection as well as humanitarian and emergency relief on equal basis among the population living within the same borders.
By : Sriprapha Petcharamesree
Date : May 29, 2020
Source : Open Democracy
https://www.opendemocracy.net/en/pandemic-border/covid-19-southeast-asia-non-citizens-have-right-protection-too/
Indigenous Mexicans turn inward to survive COVID-19, barricading villages and growing their own food
While the coronavirus hammers Mexico, some Indigenous communities in the southern Mexican state of Oaxaca are finding creative ways to cope.
Oaxaca, one of Mexico’s poorest and most ethnically diverse states, is home to numerous Indigenous communities, including the Zapotec people. I have spent many years in the central valleys of Oaxaca conducting anthropological research in rural Zapotec villages, documenting the people’s lives, migration patterns and food culture.
Now, my summer research in Oaxaca canceled due to the pandemic, I am learning from afar how the Zapotec are confronting the coronavirus given such complicating factors as chronic poverty, inadequate health care, limited internet, language barriers and a lack of running water.
Working with colleagues at Mexico’s Universidad Tecnológica de los Valles Centrales de Oaxaca and scouring online media resources, I find the Zapotec are surviving the pandemic by doing what they’ve always done when the Mexican government can’t, or won’t, help them: drawing on local Indigenous traditions of cooperation, self-reliance and isolation.
So far, it’s working. While infections and death are rising relentlessly across Mexico, many Indigenous communities in Oaxaca remain largely insulated from the coronavirus. The Indigenous Mixtec village of Santos Reyes Yucuná reported its first infection on July 17, for example – four months after COVID-19 reached Mexico.
Indigenous survival strategies
Cooperation is a cornerstone of Zapotec life in Oaxaca. A history of social exclusion by the federal government reminds the Zapotec not to rely on politicians to save them.
People work together from a young age, joining together in “tequio,” or communal labor brigades, to complete projects that can range from painting a school to repairing the electrical grid. Individuals, their families and their friends routinely work together to make small jobs go quickly and to make big jobs seem less overwhelming.
The Zapotec also maintain relative isolation from broader Mexican society, my research shows. They grow food in their “milpas,” or garden plot, to supplement store-bought fare, and police their own communities with volunteers called “topiles.” With high levels of community trust and a history of self-rule that predates the Spanish conquest, the Zapotec who continue to live in rural Oaxaca neither need nor allow much outside access to their villages.
These three aspects of traditional Zapotec culture – cooperation, isolation and self-reliance – are all helpful in a pandemic.
According to researcher M.C. Nydia Sanchez of Oaxaca’s Universidad Tecnológica, Zapotec families are sharing scarce resources like food, information, water and face masks in what’s called “guelaguetza,” the practice of working together and gift-giving.
And at a time when Mexico’s food supply chain is under stress, villagers are ensuring no one goes hungry by ramping up their crop of “maiz,” the corn used to make tortillas.
“Chapulines” – grasshoppers harvested from the fields and quickly toasted over a fire – are returning to the table as a protein-rich alternative to expensive, store-bought meats that are no longer available locally.
Consensus rules
The tight-knit nature of Zapotec communities can, however, also complicate other measures critical to limiting residents’ exposure to infection.
These are small villages of no more than a few thousand souls. Everyone knows everyone, and it is typical for Zapotec people to spend much of their day together with family and friends. This can make it difficult to maintain the social distancing recommended by national health officials.
“To no longer greet each other so much on the street [is difficult], because we are used to it,” a Zapotec man named Jose Abel Bautista Gonzalez told Reuters in April. “It is a tradition, the culture of the people.”
Rather than closing their doors to family and friends, then, the Zapotec are aiming to stop COVID-19 from getting in at all.
Across much of Oaxaca, villagers are building barricades made of chain, stones and wood to physically block access into and out of their communities, which are typically served by only one road. Many villages are effectively quarantined from society.
“We decided to set up these barriers so that visitors or outsiders wouldn’t be coming in,” José Manzano, of San Isidro del Palmar, told Global Press Journal on June 28.
Such decisions, like most Zapotec policies, are built upon community consensus – not made on the order of a local or national political leader.
Uncertain future
Indigenous Mexican communities are unlikely to escape unscathed from the pandemic.
Mexico is so far losing its battle with the economic effects of the coronavirus: Jobs are disappearing, and economists predict the national economy may contract by 8% this year. Tourism, the lifeblood of Mexico’s economy, has halted.
That means hunger and a long recession that experts say will impact the rural poor disproportionately. Mexico’s social development agency estimates up to 10 million people may fall into extreme poverty, ending the country’s nearly decade-long run of poverty reduction.
And if the coronavirus does get into Zapotec communities, it will probably hit residents hard. Their villages lack the running water, social distancing, mask supply and health care necessary to slow the spread of the disease.
The lack of potable water additionally increases the risk that intestinal problems like cholera, among other health conditions common in rural Indigenous populations, will exacerbate the effects of COVID-19.
The Mexican government has committed to build more rural hospitals, including in Oaxaca. But the virus moves faster than construction crews. The Zapotec’s best bet, they know, is still themselves.
Editor’s note: This story has been updated to accurately characterize the Indigenous inhabitants of the village Santos Reyes Yucuná.
By : Jeffrey H. Cohen (Professor of Anthropology, The Ohio State University)
Date : August 11, 2020
Source : The Conversation
https://theconversation.com/indigenous-mexicans-turn-inward-to-survive-covid-19-barricading-villages-and-growing-their-own-food-142537
Women across Latin America ‘under pressure’ to have C-sections during COVID-19
Women are facing an ‘obstetric violence’ crisis made worse by the pandemic, despite laws against mistreatment and ‘abusive medicalisation
Women giving birth across Latin America during COVID-19 have faced increasing pressure to have caesarean sections, a new investigation by openDemocracy reveals today.
The investigation also found numerous reports of mistreatment of women in labour, bans on birth companions, and refusals from medical staff to treat women during emergencies – despite laws in many countries against ‘obstetric violence’ and “abusive medicalisation”.
Latin America already had the highest rate of C-sections in the world, accounting for around 40% of its births. In contrast, the World Health Organization (WHO) recommends a rate of around 15% and insists that C-sections should happen only when medically justified.
The WHO reiterated this advice during COVID-19, in guidance published in March, stating that women should have birth companions of their choice and receive respectful treatment, clear communication, appropriate pain relief and support to breastfeed if they want to.
Performing C-sections, inductions, episiotomies and other procedures when they aren’t medically necessary, or without informed consent, is also forbidden under national or state-level laws against obstetric violence that exist in at least eight Latin American countries, including Argentina, Ecuador, Mexico, Uruguay and Venezuela.
Most of these laws also guarantee birth companions and that women can share rooms with newborns and be supported to breastfeed. But maternal health advocates say that these laws, and the WHO’s guidance, were not observed in many places even before COVID-19. Now, they say the pandemic has made things worse.
Margarita Goñi from the Birth is Ours (EPEN) advocacy group says that, during Argentina’s coronavirus lockdown in March and early April, several hospitals “started to schedule inductions or caesareans to any woman in their 38th week of pregnancy” – against ministry of health guidelines which say “it’s important to avoid unnecessary caesareans.”
Violeta Osorio, from the Las Casildas rights group, added: “Pregnant women are told a scheduled cesarean is better than going into labour at the height of a COVID outbreak. But this clashes with the need to prevent the healthcare system from being overwhelmed, as caesareans demand more resources and more days in hospital”.
In Ecuador, Sofía Benavides (also from EPEN) said that the group collected testimonies of 26 women who gave birth during COVID-19. Thirteen said they were forced to give birth ‘alone’ under restrictions that banned hospital visitors, and fifteen said they were not allowed to have early skin-to-skin contact with their babies.
Benavides also described one private clinic as “offering: ‘You come alone, get a C-section, we don’t give you a room, we keep you instead at the observation area until discharge, and charge you 1,200 dollars’. The only good thing is you would be with your baby”.
In Mexico, obstetrician Christian Mera said he expects that statistics will show a spike in caesareans in April and May driven by a “fear of overloading hospitals”. He said this fear “is inconsistent, as caesareans entail greater risks for the women, and under COVID-19 there are added risks of hospitalisation and infection.”
Bremen de Mucio, regional advisor on sexual and reproductive health for the Pan American Health Organisation/WHO told openDemocracy that across Latin America “caesareans have reached extremely high levels (even in women without COVID-19)”.
In Uruguay, which by mid-July had seen about 1,000 COVID-19 cases and around 30 deaths, the ministry of health has also been accused of turning a blind eye to hospitals dodging the law and temporarily banning companions during births.
In the Venezuelan capital Caracas, two young women who both gave birth in May in public maternity wards described feeling “alone” and “frightened” until their discharge from hospitals that had banned birth companions and other visitors under coronavirus measures.
Both told openDemocracy that they had procedures they were not consulted about, including an amniotomy (starting a woman’s labour by artificially rupturing her membranes and ‘breaking her water’), induced labour and an episiotomy (cutting a woman’s vagina).
Alone and ill-informed
Since March, openDemocracy has talked to dozens of women, maternal health advocates, midwives and obstetricians across Argentina, Ecuador, Mexico, Uruguay and Venezuela. Between them, they detailed numerous cases of childbirth during the pandemic that appear to breach both international guidelines and national laws.
Most of the women said they had to give birth without someone they knew in the room, because companions were suspended under COVID-19. This “multiplies the risks of mistreatment” in countries where “obstetric violence is always present”, warned Mexican midwife Nuria Landa, from the women’s group Nueve Lunas.
Some women also reported verbal abuse from overstretched hospital staff, while others said they were separated from their newborn babies and weren’t able to breastfeed as a result.
Breaches of the WHO guidelines and national laws have occurred in both public and private hospitals. “They didn’t treat us with dignity,” is how Lidia Cordero described giving birth without her partner in the emergency room of a public hospital in Huixquilucan, Mexico, where she said she wasn’t given adequate information about what her doctors were doing to her.
“We were literally the hospital’s plague-stricken ones,” said Montse Reyes, who had a scheduled C-section in May at a private hospital in Mexico. She says that both she and her baby tested positive for COVID-19 after the birth, but staff didn’t inform her of the test results until she was discharged following two days in isolation.
Reyes was not separated from her baby, but they were left in “an isolation area behind a glass door” and “no one was willing to be in contact with us. It was 11 pm and I’d not even had a glass of water since 10 pm the previous day.”
“I felt abandoned, with a mix of anxiety and pain,” explains Daniela Echeverría in Quito, Ecuador. While her husband was allowed in with her, she says they were left alone in a delivery room for three hours – by which point she had vaginal tearing, and her baby had swallowed amniotic fluid and meconium (signs of foetal distress).
Echeverría believes that staff numbers were reduced under COVID-19 measures, explaining how a single doctor and two nurses had to assist another birth before coming to her.
In Uruguay, Laura Vega from the NGO Grupo por la Humanización del Parto y Nacimiento said they have received 70 complaints from different parts of the country.
A lack of clear communication is a common theme throughout the testimonies gathered by openDemocracy. Two women who gave birth in different Uruguayan cities in April (before the government revoked its ban on companions in May), said they hadn’t been informed in advance that they would not be allowed to have their partners with them when they gave birth.
“I was not even told. The gynaecologist told my partner his presence was not convenient in the operating theatre,” said Anahí Oudri.
Andrea Fernández said: “I wasn’t able to argue. I was frightened by the caesarean and knew that if I didn't win the argument, it wouldn't be nice to see the staff’s angry faces.”
A global crisis
Globally, openDemocracy’s investigation has identified cases in at least 45 countries of WHO childbirth guidelines being breached since the pandemic began. The evidence comes from first-hand testimonies, NGOs and other news reports.
In Latin America, the imposition of coronavirus curfews and transport restrictions has also led to women missing antenatal check-ups, walking long distances to reach hospital, or being forced to have unplanned and risky home births.
In Venezuela in May, our reporter saw a woman who was 31 weeks pregnant initially being denied treatment by a Caracas maternity hospital. She was later transferred to another hospital, but her baby was stillborn.
In Ecuador in April, two women were repeatedly denied assistance during obstetric emergencies by public hospitals in Guayaquil, said Ana Vera, a feminist lawyer and member of the sexual and reproductive rights group Surkuna. The city was engulfed by the COVID-19 crisis at the time.
“They were assisted and given antibiotics and a life-saving transfusion only after I personally called the ministry of health,” Vera told openDemocracy.
Also in April, Nuria Landa, the midwife in Mexico, received emergency phone calls from two women who went into labour at home after they were denied help by a hospital that had been converted to a COVID-19 centre without prior warning.
Another woman in the Mexican city of Guadalajara told openDemocracy that she delivered her baby at home without complications in April, but the day after the birth she felt ill and went to a hospital for a coronavirus test (which she says was initially refused).
“The doctor put her fingers strongly inside me, revolving them,” said the woman, who described being scolded for having a home birth and told she probably had tissue in her uterus that needed to be removed. This was proven incorrect, she explained, when a second physician ordered an ultrasound – as well as a coronavirus test (which was positive).
This woman said she has reported her case to health authorities as a violation of laws against mistreatment in her state (which has not specifically criminalised obstetric violence).
It is unclear if or when these authorities will look into her complaints, and no one from ministries of health in Argentina, Ecuador, Mexico, Uruguay or Venezuela responded to openDemocracy’s requests for comment on this investigation.
Ecuador's ombudsman’s office said in May, in response to openDemocracy’s questions, that they had not received a single obstetric violence complaint during COVID-19. This office did not respond to follow-up questions for an update on this in July.
A spokesperson for the Office of the UN High Commissioner for Human Rights, Michelle Bachelet, said they have “also received reports raising concerns about the human rights of pregnant women and girls in the context of COVID-19 pandemic.”
“We are concerned that around the world, with overstretched health systems, resources for routine services, like maternal health services, are often diverted… Documenting these incidents is a critical first step to exposing the problem. States need to bring their practices in line with the WHO guidance in this area without delay.”
Additional reporting by Magda Gibelli (Venezuela) and Agostina Mileo (Argentina).
By : Diana Cariboni, Daniela Rea, Lydiette Carrion
Date : July 16, 2020
Source : Open Democracy
https://www.opendemocracy.net/en/5050/women-latin-america-pressure-c-sections-covid/
Should a COVID-19 vaccine be compulsory — and what would this mean for anti-vaxxers?
With COVID-19 vaccine developers reporting promising results, it is probable we will one day face a major public health question: can the government compel New Zealanders to be vaccinated?
Just as inevitably, some people will refuse a vaccine. As we have seen overseas with debates over the wearing of masks, and more generally with anti-vaccination activists everywhere, compulsion is not a simple matter.
There are competing rights and duties on both sides. Forcing an individual to be vaccinated is a violation of their fundamental right to personal autonomy, which informs the more specific right to bodily integrity.
Basically, those rights mean every person can make decisions for themselves and what can and cannot be done to their bodies.
The state’s duty to protect
While international human rights treaties support this, they do not specifically talk about the right to refuse medical treatment. Rather, they state that everyone has the right not to be subjected to medical experimentation without free consent.
And here we see how quickly the stakes are raised. These rights are part of the broader right to be free from torture, cruel and inhuman degrading treatment or punishment. The specific reference to medical experimentation is a response to what happened under the Nazi regime during the second world war.
But it’s the fundamental right to life that throws the COVID-19 vaccine issue into stark relief, because it also means governments must make some effort to safeguard citzens’ lives by protecting them from life-threatening diseases.
Although everyone has the right to the highest attainable standard of health, this includes the right to be free from non-consensual medical treatment. But this in turn may be subject to the state’s obligation to prevent and control disease.
The right to be free from non-consensual treatment can only be restricted under specific conditions that respect best practice and international standards.
The introduction of mass immunisation programs therefore requires quite a balancing act.
In New Zealand, the courts and their English predecessors have long recognised and protected the right to bodily integrity. The New Zealand Bill of Rights Act 1990 also clearly states that everyone has the right to refuse medical treatment.
Public health can trump individual rights
Any restriction of that right, any intrusion into the individual’s bodily integrity, would require explicit statutory authorisation. Such legislation would have to be interpreted very strictly and, wherever possible, consistently with the Bill of Rights Act.
There are examples of how this would work in practice. A recent decision from the Supreme Court of New Zealand addressed whether the fluoridation of water as a public health measure was a violation of the right to refuse medical treatment.
The court found it was. But – and it’s an important but – the court decided some public health measures could override the right to refuse medical treatment where these measures are clearly justified.
Clear justification would mean there must be a reasonable objective to compulsory vaccination that justifies the limits placed on the right to refuse medical treatment.
Such limits must be no more than are reasonably necessary to achieve the desired public health outcome, and they must be proportionate to the importance of mandatory vaccination.
Consequences for refusing vaccination?
In the end, should a COVID-19 vaccine become available, New Zealanders would have the right (but not the absolute right) under international and domestic law to refuse to be vaccinated. And the government could – and might even be obliged to – override that right.
So, no definitive answer. Furthermore, just because the government could make vaccination compulsory doesn’t mean it should.
It might not even have to. A person could still exercise their right to refuse vaccination but the government could then impose limits on other rights and freedoms.
In practical terms, this could mean no travel or access to school or the workplace if it placed the health and lives of others at risk. Similarly, a refusal to be vaccinated could limit jobs or social welfare benefits that depend on work availability.
But, again, the government would have to present clear justifications for any such restrictions.
Public consent is vital
Without a doubt, this would be highly controversial and the government would need to engage in another balancing act.
But a purely voluntary approach can have mixed results, too, as the 2019 measles outbreak showed. The main problem appears to have been a poorly designed immunisation program that missed various ethnic, socioeconomic and regional targets.
The success of a voluntary approach will be dependent on a highly performing vaccination program that is accessible to all New Zealanders and backed up by a strong public education campaign.
Ultimately, as the collective effort of the “team of 5 million” has already shown, the effectiveness of any law really depends on each one of us and the decisions we make.
By : Claire Breen (Professor of Law, University of Waikato)
Date : August 5, 2020
Source : The Conversation
https://theconversation.com/should-a-covid-19-vaccine-be-compulsory-and-what-would-this-mean-for-anti-vaxxers-143742
COVID-19 Is a Huge Threat to Stability in Africa
Ongoing conflicts — including U.S. “counterterrorism” operations — combined with escalating poverty and repression could amplify the pandemic’s social cost.
In March 2020, as the COVID-19 virus traversed the planet, UN Secretary-General António Guterres called for a global ceasefire to fight the common enemy.
The virus, compounded by the effects of armed conflict, he noted, hit the most vulnerable the hardest. Women, children, the marginalized, and the displaced were among the most defenseless. Hostilities must cease to permit the delivery of aid, the conditions for diplomacy, and ultimately, a resolution to the conflicts.
The response to Guterres’s appeal was discouraging.
Africa, a key battleground on both the pandemic and conflict fronts, had much to gain from a universal ceasefire. However, in the months that followed, little common ground emerged at negotiating tables, where weaker actors made contingent demands that the powerful refused to honor, or on the battlefields, where more powerful parties declined to lay down arms, hoping to achieve a military win.
The Security Council, divided internally, failed to endorse the proposal for more than three months. The United States posed a major obstacle when it insisted that its “counterterrorism” operations be exempted from the ban — a demand that was substantially honored in the final resolution.
Absent political will, the UN resolution will not promote the domestic and international cooperation necessary to defeat the virus. Evidence from Africa — notably, Mali, Nigeria, and Somalia — suggests that in countries already weakened by poverty, political repression, and violent extremism, the pandemic is intensifying societal tensions and exacerbating rather than quelling civil unrest.
The impact of the virus has highlighted regional inequalities. The collapse of health and economic systems, already under duress, has spurred ethnic scapegoating and xenophobia. Virus containment measures have offered authoritarian states new opportunities to strengthen their powers and repress their opponents. Internal conflicts, which before the pandemic had spilled over borders and attracted foreign military intervention, risk further intensification.
Increasing Poverty — and Risks of Extremism
African economies, already devastated by the impact of climate change, violent conflicts, and global downturns, have been further battered by the COVID-19 pandemic, which has pushed millions of people into extreme poverty.
In Mali, where 3.5 million residents face food insecurity as a result of violent extremism and civil unrest, virus-related economic shutdowns and reduced remittances may threaten 1.3 million people with hunger and impoverish 800,000 more. In Nigeria, the World Bank predicts that COVID-19 will drive oil revenues down by 70 percent this year — fallout from worldwide industrial shutdowns, work-from-home orders, and the grounding of airplanes. The ripple effects may force 5 million more residents into poverty — in a country that already tops global charts for extreme impoverishment.
Economically vulnerable populations, abandoned by their governments, are targets of opportunity for violent extremists — including many that are affiliated with al-Qaeda or the Islamic State. In Somalia, al-Shabaab has established a COVID-19 treatment center and offered protection and basic services where the state has not.
Although courted by extremists, these populations are also the extremists’ greatest victims. In northeastern Nigeria and elsewhere in the Lake Chad region, Boko Haram has refused to close its mosques and schools, rendering local populations more vulnerable to the disease. With state attention and resources diverted to the pandemic, al-Shabaab and Boko Haram have stepped up their attacks, increasing the number of internally displaced persons and refugees and provoking multinational counter-offensives that have killed countless civilians.
Scapegoating and Repression
Fear and hardship provoked by the disease have fueled a rise in ethno-nationalism, xenophobia, hate speech, and the targeting of refugees, migrants, and other marginalized populations.
Pandemic-induced border closures and movement restrictions render these populations even more vulnerable. In Yemen, where war and the COVID-19 pandemic have decimated the health system, Houthi militias have blamed migrants from Ethiopia and other parts of the Greater Horn for the virus’s spread and forced thousands into the desert without water or food. Other African migrants, pushed into Saudi Arabia, have been beaten and imprisoned.
If fear and hardship have stoked the flames, measures taken to impede the virus’s spread may generate further instability. Some governments have declared states of emergency that have broadened executive powers and opened the door to greater human rights abuses by authoritarian regimes.
Across the continent, police have violently attacked civilians who ignored lockdown rules or protested virus-induced price gouging. Informal sector workers have been disproportionately targeted, and migrants from other countries have been denied services and assistance. Elections postponed due to health concerns have allowed some leaders to extend their terms; others have used the crisis to expand their powers. In Somalia, where elections have been delayed indefinitely, opposition forces have cried foul and warned that consequences will follow.
A Recipe for Instability
The realization that we are all in this together has prompted a call for increased international cooperation to fight the COVID-19 pandemic. The UN’s call for a global ceasefire is one step in the right direction. However, the world’s response has been weak.
In Africa, warring parties and international mediators have made little progress on the diplomatic front. In Mali, Jama’at Nusrat al-Islam wal-Muslimin (JNIM), al-Qaeda’s regional affiliate, is willing to negotiate with the government — and may even collaborate against the Islamic State in Greater Sahara (ISGS). However, it will begin talks only if foreign troops depart. The powers that be have little interest in this option, and the UN resolution bolsters their position, having excluded from its ban counterterrorism operations focused on al-Qaeda, the Islamic State, and their affiliates.
The entrenchment of ethno-nationalism, xenophobia, and narrow self-interest in some of the world’s wealthiest nations makes it unlikely that the global north will commit the resources and know-how necessary to combat the virus successfully — which would eliminate one of the factors contributing to civil conflict.
While African actors on the ground are working to develop effective solutions, they are up against formidable odds. If those with power fail to act, poverty, repression, divisions within and between countries, and the long history of detrimental foreign intervention make further instability, rather than international cooperation, the most likely outcome of Africa’s COVID-19 crisis.
Elizabeth Schmidt is professor emeritus of history at Loyola University Maryland and the author of six books about Africa. Her most recent book, available for free download, is Foreign Intervention in Africa after the Cold War: Sovereignty, Responsibility, and the War on Terror.
By : Elizabeth Schmidt
Date : August 3, 2020
Source : Foreign Policy in Focus
https://fpif.org/covid-19-is-a-huge-threat-to-stability-in-africa/
U of A sociologist compiles COVID-19 stories to document extraordinary moment in history
Contributors to new website put experiences in words, music and visual art running the gamut from optimism to despair.
A University of Alberta sociologist is collecting observations, reflections and stories of COVID-19 from the public, in all formats imaginable, for a new website called Stories of the Pandemic.
The site is meant to serve as a community resource for people across the province to better understand an unprecedented time in our lives, said co-curator Amy Kaler. It aims to collect everything from short fiction and essays to diary entries, songs, photography and artwork.
“Everybody's got a story, and everybody has gone through experiences that, for good or bad, they may not have seen coming,” she said.
Diversity of experience
So far the diversity of expression has been striking, said Kaler, who is aided in her work by doctoral students Rezvaneh Erfani Hossein Pour in sociology and Subash Giri from music.Most contributors are in “descriptive mode,” hoping to capture their experience as accurately as possible and bear witness to this extraordinary moment in history.
“For those people, making sense of the pandemic amounts to really precise and realistic observation and description—using whatever form is comfortable for them,” she said.
Some prefer to analyze or generalize, explained Kaler, asking themselves, “What is this experience telling me, what is it teaching me? What do I understand now because I've been immersed in a pandemic?”
One contributor remarked on the generosity and small acts of kindness people are capable of during times of crisis, and wondered why she hadn’t appreciated it until now. Others see only the darker side of their confinement, focusing on isolation, loneliness and misery.
“One person wrote a poem describing what it feels like to be addicted to their bedroom, stuck in this one place they can never leave,” said Kaler.
Stories of the Pandemic has received a few dozen submissions so far, and Kaler said she hopes it will pick up more once people have had time to process what they’re going through.
It’s also when she expects to see more fiction and more elaborate forms of artistic expression.
“Maybe in time more people will be consciously setting out to create art, rather than using their skills to make immediate sense of the pandemic,” said Kaler.
The website has a five-year timeline before funding runs out. Eventually it will be housed in the U of A Archives, she said.
Anyone is welcome to submit as long as their work relates in some way to the pandemic experience. And though submissions are vetted before posting, Kaler said her team isn’t looking for polished work or “the perfect analysis of what's going on,” she said.
“You don't have to have everything pulled together and clearly understood, and we're open to pretty much any form that can be transmitted on the internet.”
Supported by the Faculty of Arts, Stories of the Pandemic is part of a larger “signature area” for the faculty called Stories of Change, which aims to explore “the intersection between people's individual, personal everyday lives and big social, political, economic and ecological transformation,” said Kaler.
Those interested in submitting to Stories of the Pandemic should contact Stories of Change at [email protected].
By : GEOFF McMaster
Date : July 17, 2020
Source : FOLIO
https://www.folio.ca/u-of-a-sociologist-compiles-covid-19-stories-to-document-extraordinary-moment-in-history/
The COVID-19 Gender Gap
The COVID-19 pandemic threatens to roll back gains in women’s economic opportunities, widening gender gaps that persist despite 30 years of progress.
Well-designed policies to foster recovery can mitigate the negative effects of the crisis on women and prevent further setbacks for gender equality. What is good for women is ultimately good for addressing income inequality, economic growth, and resilience.
Why has COVID-19 had disproportionate effects on women and their economic status? There are several reasons.
First, women are more likely than men to work in social sectors — such as services industries, retail, tourism, and hospitality — that require face-to-face interactions. These sectors are hit hardest by social distancing and mitigation measures. In the United States, unemployment among women was two percentage points higher than men between April-June 2020.
Because of the nature of their jobs, teleworking is not an option for many women. In the United States, about 54 percent of women working in social sectors cannot telework. In Brazil, it is 67 percent. In low-income countries, at most only about 12 percent of the population is able to work remotely.
Second, women are more likely than men to be employed in the informal sector in low-income countries. Informal employment – often compensated in cash with no official oversight – leaves women with lower pay, no protection of labor laws, and no benefits such as pensions or health insurance.
The livelihoods of informal workers have been greatly affected by the COVID-19 crisis. In Colombia, women’s poverty has increased by 3.3 percent because of the shutdown in economic activities. The UN estimates that the pandemic will increase the number of people living in poverty in Latin America and the Caribbean by 15.9 million, bringing the total number of people living in poverty to 214 million, many of them women and girls.
Third, women tend to do more unpaid household work than men, about 2.7 hours per day more to be exact. They bear the brunt of family care responsibilities resulting from shutdown measures such as school closures and precautions for vulnerable elderly parents. After shutdown measures have been lifted, women are slower to return to full employment. In Canada, the May job report shows that women’s employment increased by 1.1 percent compared with 2.4 percent for men, as childcare issues persist. Furthermore, among parents with at least one child under the age of 6, men were roughly three times more likely to have returned to work than women.
Fourth, pandemics put women at greater risk of losing human capital. In many developing countries, young girls are forced to drop out of school and work to supplement household income. According to the Malala Fund report, the share of girls not attending school nearly tripled in Liberia after the Ebola crisis, and girls were 25 percent less likely than boys to re-enroll in Guinea. In India, since the COVID-19 lockdown went into effect, leading matrimony websites have reported 30 percent surges in new registrations as families arrange marriages to secure their daughters’ futures. Without education, these girls suffer a permanent loss of human capital, sacrificing productivity growth and perpetuating the cycle of poverty among women.
It is crucial that policymakers adopt measures to limit the scarring effects of the pandemic on women. This could entail a focus on extending income support to the vulnerable, preserving employment linkages, providing incentives to balance work and family care responsibilities, improving access to health care and family planning, and expanding support for small businesses and the self-employed. Elimination of legal barriers against women’s economic empowerment is also a priority. Some countries have moved quickly to adopt some of these policies.
Austria, Italy, Portugal, and Slovenia have introduced a statutory right to (partially) paid leave for parents with children below a certain age, and France has expanded sick leave to parents impacted by school closures if no alternative care or work arrangements can be found.
Latin American women leaders have established the “Coalition of Action for the Economic Empowerment of Women” as part of a wider whole-of-government effort to increase women’s participation in the post-pandemic economic recovery.
In Togo, 65 percent of participants in a new mobile cash-transfer program are women. The program enables informal workers to receive grants of 30 percent of minimum wage.
Over the longer term, policies can be designed to tackle gender inequality by creating conditions and incentives for women to work. As discussed in a recent blog, particularly effective are gender-responsive fiscal policies, such as investing in education and infrastructure, subsidizing childcare, and offering parental leave. These policies are not only crucial to lift constraints on women’s economic empowerment, they are necessary to promote an inclusive post-COVID-19 recovery.
This blog drew from a body of work undertaken by the IMF available at the Gender and IMF page on imf.org.
By : Kristalina Georgieva, Stefania Fabrizio, Cheng Hoon Lim and Marina M. Tavares
Date : July 21, 2020
Source : IMFBlog
https://blogs.imf.org/2020/07/21/the-covid-19-gender-gap/
Why governments have the right to require masks in public
Experts say mask rules, like smoking bans, protect workers
Requirements for consumers to wear masks at public places like retail stores and restaurants are very similar to smoking bans, according to three university experts.
Writing in the American Journal of Preventive Medicine, the professors say mask requirements to stop the spread of COVID-19 should be considered “fundamental occupational health protections” for workers at stores, restaurants and other public places.
“Both tobacco smoke and COVID-19 are air-based health hazards to workers who may be exposed to them for hours on end,” said Michael Vuolo, co-author of the paper and associate professor of sociology at The Ohio State University.
“Requiring that members of the public wear masks is a form of workplace protection.”
Vuolo, who researches the effectiveness of smoking bans, wrote the article with Brian Kelly, a professor of sociology at Purdue University who is an expert on health policy, and Vincent Roscigno, a professor of sociology at Ohio State who is an expert on labor and worker rights.
The main argument typically made against a mask requirement, as was the case with smoking bans, is that it violates the individual liberties of Americans.
“But even the strictest individual liberty philosophies still recognize that those liberties only go to the point of harm against others,” Vuolo said.
“It is clear that COVID-19 is a threat to workers who may be exposed to it and mask wearing can help minimize that threat.”
The issue is also one of inequality, because many of the workers in service and retail industries are people who earn lower wages and are racial and ethnic minorities.
Mask requirements may be a key means to reduce the already evident inequalities in who gets COVID-19, the researchers said.
The risks of contracting COVID-19 for workers are, in some ways, even more insidious than those related to smoking, Vuolo noted.
“The risk from smokers is clear. But workers don’t know who may have COVID-19 and who doesn’t. That makes mask requirements for everyone even more important,” he said.
Many business owners enforce smoking bans even when not required by law for a very good reason, according to Vuolo.
“Research has shown that workplace productivity is higher in workplaces that are seen as healthy and safe.”
Vuolo said it is important to remember how controversial smoking bans were when they were first implemented. Now, they are hardly mentioned.
“No one is out there policing smoking for the most part. Health authorities could if they had to, but it is usually not necessary,” he said.
“The way we got people to stop smoking in public was simply to make it abnormal. We could do a similar thing by making it abnormal not to wear a mask,” he said.
If mask-wearing is required, it could become as normalized here in the United States as it is in east Asia. At some point, people may even consider wearing masks during normal flu seasons, Vuolo said.
But until that time, we need legal requirements to protect workers, according to the authors.
“Wearing a mask may seem like a nuisance, just like having to step outside to smoke may seem like a nuisance,” Vuolo said.
“But both are a small inconvenience when compared to workers’ rights to a safe work environment.”
By : Jeff Grabmeier ([email protected])
Date : July 16, 2020
Source : Ohio State News
https://news.osu.edu/why-governments-have-the-right-to-require-masks-in-public/
Why do some COVID-19 patients infect many others, whereas most don’t spread the virus at all?
Science’s COVID-19 reporting is supported by the Pulitzer Center.
When 61 people met for a choir practice in a church in Mount Vernon, Washington, on 10 March, everything seemed normal. For 2.5 hours the chorists sang, snacked on cookies and oranges, and sang some more. But one of them had been suffering for 3 days from what felt like a cold—and turned out to be COVID-19. In the following weeks, 53 choir members got sick, three were hospitalized, and two died, according to a 12 May report by the U.S. Centers for Disease Control and Prevention (CDC) that meticulously reconstructed the tragedy.
Many similar “superspreading events” have occurred in the COVID-19 pandemic. A database by Gwenan Knight and colleagues at the London School of Hygiene & Tropical Medicine (LSHTM) lists an outbreak in a dormitory for migrant workers in Singapore linked to almost 800 cases; 80 infections tied to live music venues in Osaka, Japan; and a cluster of 65 cases resulting from Zumba classes in South Korea. Clusters have also occurred aboard ships and at nursing homes, meatpacking plants, ski resorts, churches, restaurants, hospitals, and prisons. Sometimes a single person infects dozens of people, whereas other clusters unfold across several generations of spread, in multiple venues.
Other infectious diseases also spread in clusters, and with close to 5 million reported COVID-19 cases worldwide, some big outbreaks were to be expected. But SARS-CoV-2, like two of its cousins, severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), seems especially prone to attacking groups of tightly connected people while sparing others. It’s an encouraging finding, scientists say, because it suggests that restricting gatherings where superspreading is likely to occur will have a major impact on transmission, and that other restrictions—on outdoor activity, for example—might be eased.
“If you can predict what circumstances are giving rise to these events, the math shows you can really, very quickly curtail the ability of the disease to spread,” says Jamie Lloyd-Smith of the University of California, Los Angeles, who has studied the spread of many pathogens. But superspreading events are ill-understood and difficult to study, and the findings can lead to heartbreak and fear of stigma in patients who touch them off.
Most of the discussion around the spread of SARS-CoV-2 has concentrated on the average number of new infections caused by each patient. Without social distancing, this reproduction number (R) is about three. But in real life, some people infect many others and others don’t spread the disease at all. In fact, the latter is the norm, Lloyd-Smith says: “The consistent pattern is that the most common number is zero. Most people do not transmit.”
That’s why in addition to R, scientists use a value called the dispersion factor (k), which describes how much a disease clusters. The lower k is, the more transmission comes from a small number of people. In a seminal 2005 Nature paper, Lloyd-Smith and co-authors estimated that SARS—in which superspreading played a major role—had a k of 0.16. The estimated k for MERS, which emerged in 2012, is about 0.25. In the flu pandemic of 1918, in contrast, the value was about one, indicating that clusters played less of a role.
Estimates of k for SARS-CoV-2 vary. In January, Julien Riou and Christian Althaus at the University of Bern simulated the epidemic in China for different combinations of R and k and compared the outcomes with what had actually taken place. They concluded that k for COVID-19 is somewhat higher than for SARS and MERS. That seems about right, says Gabriel Leung, a modeler at the University of Hong Kong. “I don’t think this is quite like SARS or MERS, where we observed very large superspreading clusters,” Leung says. “But we are certainly seeing a lot of concentrated clusters where a small proportion of people are responsible for a large proportion of infections.” But in a recent preprint, Adam Kucharski of LSHTM estimated that k for COVID-19 is as low as 0.1. “Probably about 10% of cases lead to 80% of the spread,” Kucharski says.
That could explain some puzzling aspects of this pandemic, including why the virus did not take off around the world sooner after it emerged in China, and why some very early cases elsewhere—such as one in France in late December 2019, reported on 3 May—apparently failed to ignite a wider outbreak. If k is really 0.1, then most chains of infection die out by themselves and SARS-CoV-2 needs to be introduced undetected into a new country at least four times to have an even chance of establishing itself, Kucharski says. If the Chinese epidemic was a big fire that sent sparks flying around the world, most of the sparks simply fizzled out.
Why coronaviruses cluster so much more than other pathogens is “a really interesting open scientific question,” says Christophe Fraser of the University of Oxford, who has studied superspreading in Ebola and HIV. Their mode of transmission may be one factor. SARS-CoV-2 appears to transmit mostly through droplets, but it does occasionally spread through finer aerosols that can stay suspended in the air, enabling one person to infect many. Most published large transmission clusters “seem to implicate aerosol transmission,” Fraser says.
Individual patients’ characteristics play a role as well. Some people shed far more virus, and for a longer period of time, than others, perhaps because of differences in their immune system or the distribution of virus receptors in their body. A 2019 study of healthy people showed some breathe out many more particles than others when they talk. (The volume at which they spoke explained some of the variation.) Singing may release more virus than speaking, which could help explain the choir outbreaks. People’s behavior also plays a role. Having many social contacts or not washing your hands makes you more likely to pass on the virus.
The factor scientists are closest to understanding is where COVID-19 clusters are likely to occur. “Clearly there is a much higher risk in enclosed spaces than outside,” Althaus says. Researchers in China studying the spread of the coronavirus outside Hubei province—ground zero for the pandemic—identified 318 clusters of three or more cases between 4 January and 11 February, only one of which originated outdoors. A study in Japan found that the risk of infection indoors is almost 19 times higher than outdoors. (Japan, which was hit early but has kept the epidemic under control, has built its COVID-19 strategy explicitly around avoiding clusters, advising citizens to avoid closed spaces and crowded conditions.)
Some situations may be particularly risky. Meatpacking plants are likely vulnerable because many people work closely together in spaces where low temperature helps the virus survive. But it may also be relevant that they tend to be loud places, Knight says. The report about the choir in Washington made her realize that one thing links numerous clusters: They happened in places where people shout or sing. And although Zumba classes have been connected to outbreaks, Pilates classes, which are not as intense, have not, Knight notes. “Maybe slow, gentle breathing is not a risk factor, but heavy, deep, or rapid breathing and shouting is.”
Probably about 10% of cases lead to 80% of the spread.
-Adam Kucharski, London School of Hygiene & Tropical Medicine
Timing also plays a role. Emerging evidence suggests COVID-19 patients are most infectious for a short period of time. Entering a high-risk setting in that period may touch off a superspreading event, Kucharski says; “Two days later, that person could behave in the same way and you wouldn’t see the same outcome.”
Countries that have beaten back the virus to low levels need to be especially vigilant for superspreading events, because they can easily undo hard-won gains. After South Korea relaxed social distancing rules in early May, a man who later tested positive for COVID-19 visited several clubs in Seoul; public health officials scrambled to identify thousands of potential contacts and have already found 170 new cases.
If public health workers knew where clusters are likely to happen, they could try to prevent them and avoid shutting down broad swaths of society, Kucharski says. “Shutdowns are an incredibly blunt tool,” he says. “You’re basically saying: We don’t know enough about where transmission is happening to be able to target it, so we’re just going to target all of it.”
But studying large COVID-19 clusters is harder than it seems. Many countries have not collected the kind of detailed contact tracing data needed. And the shutdowns have been so effective that they also robbed researchers of a chance to study superspreading events. (Before the shutdowns, “there was probably a 2-week window of opportunity when a lot of these data could have been collected,” Fraser says.)
The research is also prone to bias, Knight says. People are more likely to remember attending a basketball game than, say, getting a haircut, a phenomenon called recall bias that may make clusters seem bigger than they are. Clusters that have an interesting social angle—such as prison outbreaks—may get more media coverage and thus jump out to researchers, while others remain hidden. Clusters of mostly asymptomatic infections may be missed altogether.
Privacy is another concern. Untangling the links between patients can reveal who was at the origin of a cluster or expose information about people’s private lives. In its report about the chorus, CDC left out a seating map that could show who brought the virus to the practice. Some clubs involved in the new South Korean cluster were gay venues, which resulted in an antigay backlash and made contact tracing harder.
Fraser, who is tracking HIV transmission in Africa by sequencing virus isolates, says it is a difficult trade-off, but one that can be managed through good oversight and engagement with communities. Epidemiologists have “a duty” to study clusters, he says: “Understanding these processes is going to improve infection control, and that’s going to improve all of our lives.”
Kai is a contributing correspondent for Science magazine based in Berlin, Germany. He is the author of a book about the color blue, published in 2019.
By : Kai Kupferschmidt
Date : May 19, 2020
Source : ScienceMag.org
https://www.sciencemag.org/news/2020/05/why-do-some-covid-19-patients-infect-many-others-whereas-most-don-t-spread-virus-all
Is there more than one strain of the new coronavirus?
Since the emergence of the new coronavirus, called SARS-CoV-2, several researchers have proposed that there is more than one strain, and that mutations have led to changes in how infectious and deadly it is. However, opinions are divided.
Genetic mutations are a natural, everyday phenomenon. They can occur every time genetic material is copied.
When a virus replicates inside the cell it has infected, the myriad of new copies will have small differences. Why is this important?
When mutations lead to changes in how a virus behaves, it can have significant consequences. These do not necessarily have to be detrimental to the host, but in the case of vaccines or drugs that target specified viral proteins, mutations may weaken these interactions.
Since the emergence of SARS-CoV-2, several research studies have highlighted variations in the virus’s genetic sequence. This has prompted discussion about whether or not there are several strains, if this has an impact on how easily the virus can infect a host, and whether or not this affects how many more people are likely to die.
Many scientists have called for caution. In this Special Feature, we summarize what researchers currently know about SARS-CoV-2 mutations and hear from experts about their views on what these mean for the pandemic.
Why are mutations significant?
SARS-CoV-2 is an enveloped RNA virus, which means that its genetic material is encoded in single-stranded RNA. Inside a host cell, it makes its own replication machinery.
RNA viruses have exceptionally high mutations rates because their replications enzymes are prone to errors when making new virus copies.
Virologist Prof. Jonathan Stoye, a senior group leader at the Francis Crick Institute in London in the United Kingdom, told Medical News Today what makes virus mutations significant.
“A mutation is a change in a genetic sequence,” he said. “The fact of a mutational change is not of primary importance, but the functional consequences are.”
If a particular genetic alteration changes the target of a drug or antibody that acts against the virus, those viral particles with the mutation will outgrow the ones that do not have it.
“A change in a protein to allow virus entry into a cell that carries very low amounts of receptor protein could also provide a growth advantage for the virus,” Prof. Stoye added.
“However, it should be stressed that only a fraction [of] all mutations will be advantageous; most will be neutral or harmful to the virus and will not persist.”
“Mutations in viruses clearly do matter, as evidenced by the need to prepare new vaccines against [the] influenza virus every year for the effective prevention of seasonal flu and the need to treat HIV-1 simultaneously with several drugs to [prevent the] emergence of resistant virus.” – Prof. Jonathan Stoye
Researchers find mutations
MNT recently featured a research study by a team from Arizona State University in Tempe. The paper described a mutation that mimics a similar event that occurred during the SARS epidemic in 2003.
The team studied five nasal swab samples that had a positive SARS-CoV-2 test result. They found that one of these had a deletion, which means that a part of the viral genome was missing. To be precise, 81 nucleotides in the viral genetic code were gone.
Previous research indicated that similar mutations lowered the ability of the SARS virus to replicate.
Another study, this time in the Journal of Translational Medicine, proposed that SARS-CoV-2 had picked up specific mutation patterns in distinct geographical regions.
The researchers, from the University of Maryland in Baltimore and Italian biotech company Ulisse Biomed in Trieste, analyzed eight recurrent mutations in 220 COVID-19 patient samples.
They found three of these exclusively in European samples and another three exclusively in samples from North America.
Another study, which has not yet been through the peer review process, suggests that SARS-CoV-2 mutations have made the virus more transmissible in some cases.
In the paper, Bette Korber — from the Los Alamos National Laboratory in New Mexico — and collaborators describe 13 mutations in the region of the viral genome that encodes the spike protein.
This protein is crucial for infection, as it helps the virus bind to the host cell.
The researchers note that one particular mutation, which changes an amino acid in the spike protein, “may have originated either in China or Europe, but [began] to spread rapidly first in Europe, and then in other parts of the world, and which is now the dominant pandemic form in many countries.”
Prof. Stoye commented that the results of this study are, in some ways, not surprising.
“Viruses are typically finely tuned to their host species. If they jump species, e.g., from bat to human, a degree of retuning is inevitable both to avoid natural host defenses and for optimum interaction with the cells of the new host,” he said.
“Random mutations will occur, and the most fit viruses will come to predominate,” he added. “Therefore, it does not seem surprising that SARS-CoV-2 is evolving following its jump to, and spread through, the human population. Clearly, such changes are currently taking place, as evidenced by the apparent spread of the [mutation] observed by Korber [and colleagues].”
However, Prof. Stoye does not think that it is clear at this point how mutations will drive the behavior of SARS-CoV-2 in the long term.
“Fears about SARS-CoV-2 evolution to resist still-to-be-developed vaccines and drugs are not unreasonable,” he explained. “Nevertheless, it is also possible that we will see evolution to a less harmful version of the virus, as may well have occurred following initial human colonization by the so-called seasonal coronaviruses.”
Opinions remain divided
Earlier this year, researchers from Peking University in Beijing, China, published a paper in National Science Review describing two distinct lineages of SARS-CoV-2, which they termed “S” and “L.”
They analyzed 103 virus sequence samples and wrote that around 70% were of the L lineage.
However, a team at the Center for Virus Research at the University of Glasgow in the U.K. disagreed with the findings and published their critique of the data in the journal Virus Evolution.
“Given the repercussions of these claims and the intense media coverage of these types of articles, we have examined in detail the data presented […] and show that the major conclusions of that paper cannot be substantiated,” the authors write.
Prof. David Robertson, head of Viral Genomics and Bioinformatics at the Centre for Virus Research, was part of the team. MNT asked his views on the possibility of there being more than one strain of SARS-CoV-2.
“Until there is some evidence of a change in virus biology, we cannot say that there are new strains of the virus. It’s important to appreciate that mutations are a normal byproduct of virus replication and that most mutations we observe won’t have any impact on virus biology or function,” he said.
“Some of the reports of, for example, amino acid changes in the spike protein are interesting, but at the moment, these are at best a hypothesis. Their potential impact is currently being tested in a number of labs.”
Prof. Stoye thinks that it is “more a case of semantics rather than anything else” at the moment.
“If we have different sequences, we have different strains. Only when we have a greater understanding of the functional consequences of the evolutionary changes observed does it make sense to reclassify the different isolates,” he said.
“At that point, we can seek to correlate sequence variation with prognostic or therapeutic implications. This may take a number of years.”
Serotypes and future research
So, what kind of evidence are skeptical scientists looking for in the debate around multiple SARS-CoV-2 strains?
MNT asked Prof. Mark Hibberd, from the London School of Hygiene and Tropical Medicine in the U.K., to weigh in on the debate.
“For virologists, ‘strain’ is rather a subjective word that does not always have a clear specific meaning,” he commented.
“More useful in the SARS-CoV-2 situation would be the idea of ‘serotype,’ which is used to describe strains that can be distinguished by the human immune response — an immune response to one serotype will not usually protect against a different serotype. For SARS-CoV-2, there is no conclusive evidence that this has happened yet.”
“To show that the virus has genetically changed sufficiently to create a different immune response, we would need to characterize the immune protection and show that it worked for one serotype and not for another,” he continued.
Prof. Hibberd explained that scientists are studying neutralizing antibodies to help them define a serotype for SARS-CoV-2. These antibodies can prevent the virus from infecting a host cell, but they may not be effective against a new strain.
“Several groups around the world have identified a specific mutation in the SARS-CoV-2 spike protein, and they are concerned that this mutation might alter this type of binding, but we cannot be sure it does that at the moment. More likely, this mutation will likely affect the virus binding to its receptor […], which might affect transmissibility.”– Prof. Mark Hibberd
“We ideally need experimental evidence, [such as a] demonstration of a mutation leading to a functional change in the virus in the first instance, and secondly a demonstration that this change will have an impact in [people with the infection],” Prof. Robertson suggested.
He pointed to lessons that experts learned during the 2014–2018 Ebola outbreak in West Africa, where several research groups had suggested that a mutation had resulted in the virus becoming more easily passed between people and more deadly.
Cell culture experiments showed that the mutated virus was able to replicate more rapidly. However, when scientists subsequently studied this in animal models, they found that it did not behave any differently than stains without the mutation.
Scientists around the world continue to search for answers to the many outstanding questions around SARS-CoV-2. No doubt, we will see more research emerge in the coming months and years that will assess the impact of SARS-CoV-2 mutations on the COVID-19 pandemic and the future of this new coronavirus.
By : Yella Hewings-Martin, Ph.D.
Fact checked : Jasmin Collier
Date : May 22, 2020
Source : Medical News Today
https://www.medicalnewstoday.com/articles/is-there-more-than-one-strain-of-the-new-coronavirus
Will Covid-19 show us how to design better cities?
Around the world, cities are cleaner and quieter. Can we reinvent them – and ensure that the changes forced upon them in the last few months are not squandered?
Covid-19 has changed the way that towns and cities look. It has offered views of public places with fewer cars and cleaner air, roads you can stroll down, cycling without danger. It has made some things seem more precious, such as green spaces and parks. It has renewed appreciation of the social infrastructures of support and care. It has heightened awareness of the ways in which one person’s actions can affect another’s. It has made everyone more conscious of the ways they occupy space in relation to other people.
It has also prompted the idea that big cities have taken a hit from which they won’t fully recover. The virus first appeared in Wuhan, population 11 million, and some of its worst outbreaks have been in New York, London, Milan and São Paulo. Crowds and public transport, goes the theory, are bad for your health. Remote working, boosted by lockdowns, will be here to stay. Balaji Srinivasan, a Silicon Valley venture capitalist summed this view up in a pithy tweet: “Sell city, buy country.”
So cities appear both more and less attractive. It’s a contradiction. To which the best response might not be a rush away from everything urban, but a less violent redistribution from one kind of city to another. For several decades wealth and population have been tending to concentrate in a few privileged urban centres, to the disadvantage both of other towns and cities – and of themselves. This has been particularly true in Britain, with its gross imbalance between London and its satellites and much of the rest of the country. What if there were a shift in intensity away from the biggest cities towards the others, such that the enjoyment of life was increased all round?
Much or most of the lockdown’s changes are temporary. But what if this crisis were not allowed to go to waste? What if the glimpses of alternative realities became guides to the future? There have already been some rapid responses both in Britain and elsewhere, such as the closing of several central London streets to traffic by mayor Sadiq Khan, the pedestrianisation of Grey Street in Newcastle and the permanent closure of Seattle streets that had been temporarily blocked.
These initiatives are welcome attempts to make selected urban areas more sociable and pleasurable. There is also the chance to steer the decentralising effects of the pandemic towards towns and cities that already have most of what it takes to support successful communities, but could do with a bit more economic and social energy. This is surely preferable to a flight towards car-dependent detached houses, scattered around rural areas that would hardly welcome them.
Some situations that were under strain before the virus have been revealed as all-but unsupportable. In the capital, there was scarce and expensive housing, air pollution, long commuting times on crowded public transport. Lockdown has made confined living conditions less tolerable while also removing the compensations of a metropolitan social life.
Elsewhere there was a lack of investment and opportunity, alongside decaying buildings and public spaces. A three-bedroom Victorian terraced house in Fulham, to take property prices as a measure, goes for at least £1m. An essentially identical house in Gateshead might sell for £100,000, in Portsmouth maybe £250,000. London is overcrowded, Doncaster is depopulated. Empty space is at a premium in the capital and in its south-eastern penumbra. In high streets across the country there is all too much of it.
Meanwhile attempts to mitigate the London-centred housing crisis have foundered on familiar rocks. Residents of green belts don’t want new homes near them. Almost any land inside London that is easy to develop has been built on by now. Property companies can’t and won’t build homes of the quantity and affordability that are needed. There are ways to confront these problems – good planning, state housebuilding, some determination – which shouldn’t be abandoned, but contemporary Britain has so far proved sluggish to adopt them.
Another approach is to make best use of the already-there. Ease the pressure on London and on some other mostly southern hotspots and reflate the many towns and cities that often have good housing stock, handsome if neglected high streets, a legacy of past investment in public amenities like parks and libraries, and access to beautiful countryside. Places roughly answering this description include Preston, Walsall, Sheffield, Plymouth, Colchester, Derby, Dundee, Hull, Wakefield and Wrexham, to name but a few. Such a shift would have the added environmental benefit of reducing the large costs in energy and carbon of a mass housebuilding programme.
It’s been widely pointed out, especially since the pandemic started, that modern attitudes to cities have been closely linked to health. A century or so ago, for planning theorists from Ebenezer Howard to Le Corbusier, diseases such as tuberculosis made density a killer, and so cities had to be depopulated, their teeming streets replaced with green open spaces. Patrick Abercrombie’s Greater London Plan of 1944 put these ideas into practice, directing that a large number of Londoners should be moved to healthy new towns.
Once antibiotics had pushed back TB, the virtues of city life were reasserted. Jane Jacobs celebrated these virtues in The Death and Life of Great American Cities of 1961, after which it became the creed of right-thinking urbanists that the density and vibrancy of cities were to be encouraged. Theory was eventually put into practice with spectacular success, at least in economically powerful and good-looking cities including London and New York.
Populations started growing after decades of decline, money poured in, shops and restaurants boomed, property prices soared, derelict buildings were done up. The 1980s phrase “inner-city deprivation” gave way to the estate agents’ buzz-term “urban lifestyle”. The term “world cities” came into use in the 1990s, to describe urban economies that were competing with rivals of a global scale for business and attractiveness. Cities were good. Big was good. Big cities were best.
In the process something was lost. Supercharged property prices turned cities’ best features into commodities. If Jacobs talked of the “ballet of the street” – the choreography of people of different backgrounds and trades going about their lives in shared spaces – it became hard to find in the sealed glass towers of the world cities’ newest real estate. It is more likely to be found in, well, streets, of which there are countless numbers across the country, not just in the most privileged metropolitan centres.
So the proposition is not to rush from dense city to atomised exurb. Rather it is to encourage an adjustment of priorities towards towns and cities in general. It is not about mass internal migration but about incremental change. Most people will stay where they are. Most people’s lives will not be transformed by remote working. But for at least some people, some of the time, the advantages of online interactions will outweigh the disadvantages. It might mean that you only need to visit a big-city office once a week, for example, rather than every day.
It should be possible to imagine that Person A decides that the possibility of having a house and a garden outweighs the attractions of the big city. The development of remote working makes this a little more possible. Perhaps there are enough people like her to form a social network in her area, perhaps she persuades some friends to join her. Their choices might be influenced by the rediscovery, during the lockdown, of activities that don’t require a sophisticated urban pleasure dome within easy reach: cooking, talking to family or friends, going to shops that are not supermarkets, tending a garden, online socialising and entertainment. They might be less driven than before by the prestige and desirability of a metropolis.
Perhaps they work for companies who see the benefits of helping their employees live like this, or who spread their operations around regional bases more than they would have done previously. Perhaps they make an empty shop into a shared workspace and meeting place. A cafe, you could call it. Perhaps this helps to bring some life back to a high street. They would not be moving into a void, but into an existing set of businesses and activities, with which they could be mutually supportive.
Such a shift won’t happen all by itself. Successful high streets, as the Centre for Cities thinktank has shown, are symptoms of more general strengths in local economies. Brighton, York and Cambridge were doing just fine before the pandemic, and are the most likely places to bounce back; Newport, Bradford and Wigan less so. It will, as well as the resourcefulness of individuals and companies, require some positive contributions from government.
Partly this would be a matter of supporting those things that support quality of life – parks, nurseries, street maintenance. Reversing austerity, you could call it. Partly it would be a case of investing in local transport systems and broadband. It would require creative use of the planning system – not just allowing individuals to convert shops into homes, which can create poor homes and inactive streets, but encouraging initiatives that work out new futures for whole streets at a time. Vacant shopping centres should be taken into public ownership so that, as happened with empty docklands in the 1980s, they can be made available to whoever might make the most of them. Versions of Tainan Spring in Taiwan, where an old shopping mall was made into a water garden, could be realised in Britain.
The vast financial and environmental costs of projects like HS2 and Heathrow’s third runway, together with the long time they will take to deliver any kind of return, now look – in a future that will definitely be poorer than expected – preposterous. Their main effect would be to bring more people from less-favoured parts of the country to the more favoured. It would be far better to spend the tens of billions they require on local and regional projects. Rather than bring people to where the work is, the plan should be to bring work to people, wherever they are.
This is hardly a new idea. Its most recent manifestation has been the Conservative party’s policy of “levelling up” the British regions. Last year the government launched a future high streets fund as a gesture in this direction, although its £1bn budget is very much smaller than the sums previously extracted through austerity. The overheating of London has already been causing people to live further out – commuters using improved trains from Rugby, creatives relocating to Margate. These changes might be seen as the enlargement of London’s orbit, but they at least tend towards greater decentralisation.
Other future developments might help this transfer of energy from world cities to urban settlements in general. Cars that are both driverless and electric could, for example, by using road space in a more efficient and less polluting way, allow urban density without centralised public transport systems. A virus can’t change city planning all by itself, but it can be used as a chance to push changes whose time has come.
By : Rowan Moore
Date : May 24, 2020
Source : The Guardian
https://www.theguardian.com/society/2020/may/24/will-covid-19-show-us-how-to-design-better-cities
COVID-19 has blown away the myth about ‘First’ and ‘Third’ world competence
One of the planet’s – and Africa’s – deepest prejudices is being demolished by the way countries handle COVID-19.
For as long as any of us remember, everyone “knew” that “First World” countries – in effect, Western Europe and North America – were much better at providing their citizens with a good life than the poor and incapable states of the “Third World”. “First World” has become shorthand for competence, sophistication and the highest political and economic standards.
So deep-rooted is this that even critics of the “First World” usually accept it. They might argue that it became that way by exploiting the rest of the world or that it is not morally or culturally superior. But they never question that it knows how to offer (some) people a better material life. Africans and others in the “Third World” often aspire to become like the “First World” – and to live in it, because that means living better.
So we should have expected the state-of-the-art health systems of the “First World”, spurred on by their aware and empowered citizens, to handle COVID-19 with relative ease, leaving the rest of the planet to endure the horror of buckling health systems and mass graves.
We have seen precisely the opposite.
Fatal errors
“First World” is often code for countries run by Europeans or people of European descent; some of the worst health performers on the globe in recent weeks have been “First World”. For Anglophone Africans, it is doubly interesting that two of the greatest failures in handling COVID-19 are the former coloniser, Britain, and the English-speaking superpower, the United States of America.
Both countries’ national governments have made just about every possible mistake in tackling COVID-19.
They ignored the threat. When they were forced to act, they sent mixed signals to citizens which encouraged many to act in ways which spread the infection. Neither did anything like the testing needed to control the virus. Both failed to equip their hospitals and health workers with the equipment they needed, triggering many avoidable deaths.
The failure was political. The US is the only rich country with no national health system. An attempt by former president Barack Obama to extend affordable care was watered down by right-wing resistance, then further gutted by the current president and his party. Britain’s much-loved National Health Service has been weakened by spending cuts. Both governments failed to fight the virus in time because they had other priorities.
And yet, in Britain, the government’s popularity ratings are sky high and it is expected to win the next election comfortably. The US president is behind in the polls but the contest is close enough to make his re-election a real possibility. Can there be anything more typically “Third World” than citizens supporting a government whose actions cost thousands of lives?
Western European countries such as Spain, Italy and Africa’s other wholesale coloniser, France, also battled to contain the virus. Some European countries have coped reasonably well, as have some run by the descendants of Europeans such as New Zealand and Australia. But the star performers are not in the historical “First World”.
Effective responses
The most effective response was probably South Korea’s, followed by other East Asian states and territories. This is partly because they are used to dealing with coronavirus outbreaks. But it is also because they learned from experience: South Korea’s success is due to very effective testing and tracing of infected people. Whatever the reason, it is East Asia, not “the West”, which has done what the “First World” is expected to do.
Some would reply that East Asia is now “First World”. So, it is still superior; it has simply changed its address. This is debatable. But, even if it is accepted, some places have contained the virus in distinctly “Third World” conditions.
Kerala was the first Indian state to encounter the virus but has kept deaths down to three. It had largely curbed COVID-19 but is now dealing with nearly 200 cases, all people arriving from other parts of India. Judging by its record so far, it will contain this outbreak too.
Kerala, too, has learnt from handling previous epidemics. It also has a strong health system. But one of its key tools is citizen participation: it has worked with neighbourhood watches and citizen volunteers to track the contacts of infected people. Students were recruited to build kiosks at which citizens were tested. Kerala also had the capacity to ensure that all children entitled to school meals received them after schools were closed: non-governmental organisations were mostly responsible, emphasising the partnership between the government and citizens.
Kerala’s performance is not a fluke: it has, for years, produced better health outcomes and literacy rates than the rest of India.
Nor has Africa’s response to the virus confirmed prejudices. When COVID-19 began spreading, it became almost routine for reports, commentaries – and Melinda Gates, who, with her husband Bill, heads the couple’s development foundation – to predict that Africa would be engulfed in death as the virus ripped through its weak health systems. This is, after all, what is meant to happen in the “Third World” and particularly in Africa, which is always considered the least capable continent on the planet.
So far, it has not happened. It still might but, even if it does, some countries are coping better than the dire predictions claimed (and, perhaps, better than the “First World”). One stand-out is Senegal, which has devised a cheap test for the virus and has used 3-D printing to produce ventilators at a fraction of the going price. Africa, too, has experienced recent outbreaks, notably of Ebola, and seems to have learned valuable lessons from them.
Inspiring
The “First World” is still far richer than the rest of the planet and may well remain so. So its politicians, academics and journalists will probably still believe they are better than the rest.
But the COVID-19 experience may just trigger new thinking in the “Third World”. The most basic function of a government is to protect the safety of its citizens. Ensuring that people remain healthy is at least as important a guarantee of safety as protecting them from violence.
Reasonable people would surely much rather be living in Kerala or Senegal (or East Asia) right now than in Europe and North America, raising obvious questions about who really does offer a better life.
That should inspire Africans and others in the “Third World” to ask themselves whether it makes sense to want to be America, Britain or France. COVID-19 has made a strong argument for wanting to be East Asia – or, given Africa’s circumstances, Kerala.
By : Steven Friedman (Professor of Political Studies, University of Johannesburg)
Date : May 13, 2020
Source : The Conversation
https://theconversation.com/covid-19-has-blown-away-the-myth-about-first-and-third-world-competence-138464
How COVID-19 is amplifying gender inequality in India
Women are bearing a disproportionate amount of the burden that the imposition of lockdowns, shrinking of economic opportunity has created.
While much of COVID-19’s epidemiology remains shrouded in mystery, we know that it claims the lives of men more than women — at double the rate in some countries. Other coronavirus outbreaks, such as the 2003 SARS and 2012 MERS epidemics, were also more deadly for men than women.
But this epidemiological fact risks obscuring another gender dimension of the pandemic. While men’s immune systems may be less equipped to fight the virus, the socio-economic consequences of COVID-19 are stacking the deck against women. These effects are clearest in developing countries like India, where gender inequality is a persistent challenge. Follow lockdown 4.0 guidelines live updates
Our research on the virus’s impact in slum communities in Mumbai, India’s financial capital and the biggest COVID-19 hotspot, is revealing the ways in which lockdowns exacerbate the marginalisation of women, especially poor women.
Even in normal times, women face extra burdens when infrastructure is inadequate. According to Sitaram Shelar of Pani Haq Samiti, a non-profit focused on water access, about 4.5 million people in Mumbai lack access to a household water connection, forcing them to line up at community water taps. In her 2012 award-winning book Behind the Beautiful Forevers, Katherine Boo writes: “[S]he lost two hours of her morning standing in line for water at a dribbling tap…” The operative word here is she; this task almost always falls to women.
Under India’s strict COVID-19 lockdown, household water needs have swelled, owing to high summer temperatures, all family members being at home, and the emphasis on frequent hand-washing. The result: Women are spending more time queuing up. Some are also turning to an underground water market, which operates under the cloak of darkness. Shelar explained that as women step out in the wee hours of the morning to buy water, they often face sexual and verbal harassment. Follow Covid India live updates
Harassment, however, is mostly escalating behind closed doors. Aparna Joshi, Project Director of iCall, a mental health helpline, called the current situation “a brewing pot”. Frustrated, unemployed, and/or struggling to access tobacco and alcohol, several men are unloading their anger through physical, verbal and sexual assault. The surge of violence is affecting millions of women of all classes.
Some non-profits in India are finding creative tactics to support women, like hiding phone numbers for domestic abuse hotlines inside food rations. Yet, these laudable efforts pale in comparison to the scale of the challenge. The UNFPA warns that the pandemic could reduce progress against gender-based violence by one-third.
COVID-19 is shifting other household dynamics, too. Domestic responsibilities that women bear, like cooking and cleaning, have ballooned. Even worse, because women in Indian families tend to eat last and the least, research has shown that financial strain and food shortages affect women’s nutrition more than men’s. The same pattern is visible across the developing world, from Zimbabwe to Bangladesh.
To make matters worse, the lockdown has cut off most formal and informal support systems for women. In developing countries, low-income families often share one smartphone, owned by the husband. According to Joshi, women’s lack of digital access is making them more vulnerable to misinformation.
Unequal access to technology will fuel other consequences for women — especially in education and employment. As many of the world’s children switch to online learning, girls in countries like India may lose out, given that they are less likely than boys to have access to the internet. And as analysts foresee more jobs moving online post-pandemic, the digital divide might exacerbate job market inequalities.
In fact, many aspects of the COVID-19 economic fallout are likely to reduce job prospects for women.
As India eases its lockdown with requirements that businesses operate with fewer employees, trends toward mechanisation could accelerate. Because women are generally relegated to menial tasks within production processes, their jobs are often the first to go when firms automate. And with partial lockdowns involving reduced public transit, women might find their access to work curtailed, given their disproportionate reliance on buses and trains for commuting.
India already struggles with declining female labour force participation — on par with Saudi Arabia at 24 per cent. If women’s employment continues to drop post-COVID, this will only magnify the damage to their position in families and society, given that employment is one of the strongest predictors of women’s empowerment, not to mention important for boosting GDP.
What would a gender-sensitive pandemic response look like? It begins with a full-throttled focus on supporting women who face domestic violence. A recent court ruling in Delhi provides a roadmap: Publicising helplines, relaxing lockdown rules for women to leave home and seek support, and sensitising the police.
And women’s employment must become a priority in recovery efforts. Initiatives to enhance digital access and skills should be scaled up and targeted specifically to low-income women. Direct employment programmes to provide necessary supplies should be expanded; for example, the government in the state of Andhra Pradesh is employing thousands of women to stitch masks.
Not only in India, but in every part of the world, the social and economic crisis of COVID-19 must be understood through the lens of gender. The policy response must be structured around rebuilding economies and societies in ways that empower women to lead safe, productive and fulfilling lives.
Shah is a senior associate at IDFC Institute, a think tank in Mumbai, Gandhi a visiting scholar at Brookings India and is a postdoctoral scholar at the Lusk Center for Real Estate at the University of Southern California and Randolph is founding partner of the JustJobs Network and a PhD candidate in urban planning at the University of Southern California
By : Kadambari Shah, Sahil Gandhi, and Gregory Randolph
Date : May 17, 2020
Source : India Express
https://indianexpress.com/article/opinion/coronavirus-gender-inequality-india-6414659/
Covid-19 hurts the most vulnerable – but so does lockdown. We need more nuanced debate
The class and racial consequences of this crisis mean we must think more carefully about how we ‘reopen’ the economy
The argument over lockdown seems to have crystallized into a simple – and simplistic – binary: health versus the economy. If you position yourself on the left, you value health over money, and so support the lockdown. That’s a mistake.
The “health versus the economy” frame ignores how disastrous the lockdown has been to America’s poor. Despite rhetoric about “shared sacrifice”, the ability to self-isolate is overwhelmingly correlated to income. While middle-class professionals congratulate themselves for staying inside, their isolation is dependent on a class of workers who often labor without essential equipment or while ill. Making matters worse, these exposed workers also tend to have more of the health conditions – including hypertension and diabetes – that make Covid-19 so deadly. In America, getting sick is a class condition.
This pandemic is an X-ray, exposing the racial and class inequalities of our society. Look at the data on the communities that are hardest hit by the virus. New York City is often described as the “center of the pandemic”, but a map of the most affected areas clearly shows that poorer neighborhoods are bearing the brunt. In Chicago, 70 of the first 100 Covid-19 victims were black; Milwaukee tells a similar story.
To make matters worse, the government’s measures to mitigate the economic effects of Covid-19 lockdowns exacerbate previously existing inequalities. Trump’s much-vaunted bailout has created a multitrillion-dollar money supply for the largest corporations in the country, with almost no critical oversight requirements. At the same time, people whose livelihoods are being destroyed are being asked to make do with a one-off $1,200 payment, the conditions for which exclude many of those who need it most.
This amounts to a massive transfer of wealth from the poor to the rich. Just like in 2008, capital has taken hold of the crisis, and turned it to its own advantage.
Yet at this stage simply lifting the lockdown to get the economy going would do more harm than good. The lockdown has generated its own crisis. Immediately lifting the lockdown would risk exacerbating the damage already suffered by America’s poorest.
In April, at least 20 million people filed for unemployment. The sectors most affected by these job losses – those predicated on face-to-face interaction – are overwhelmingly peopled by precariously employed, low-paid laborers who have little in the way of savings or capacity to weather this catastrophe. The lockdown thus doubly damns the poor: most likely to be made ill at work, they are also most likely to lose their jobs.
That doesn’t mean it makes sense to rush people back to work in unsafe conditions that might lead to a new spike of infections. Many workers are rightly scared of returning to workplaces that do not properly ensure their safety. Given the intense competition that is likely to emerge over the few jobs that remain in America, many big employers may create a “race to be bottom” that forces workers to compete to accept dangerous working conditions.
Taking the class and racial consequences of this crisis seriously means thinking more carefully about how we “reopen” the economy.
One way to do this would have been a program of contact tracing, aimed at identifying, isolating and taking care of those who actually have the disease (or are most vulnerable to it), while allowing others to keep the economy going. Such a program was successfully undertaken in South Korea. Unfortunately, it may already be too late for this approach. In any event, Trump’s Republican base would never tolerate what they view as a violation of privacy.
The strategy adopted by some northern European countries – such as Sweden – was another possibility. Keeping the economy going, while offering quality healthcare and other benefits to those who get sick, is less irrational than it might seem. That approach involves less economic disruption. Whether it leads to more deaths in the long run is still an open question. The problem is that the Swedish model pre-supposes a well-functioning healthcare system, whereas American healthcare has suffered decades of contraction under the brunt of neoliberal policies; South Korea has three times as many hospital beds per 1,000 people as the US does.
Neither the Swedish nor South Korean models are possible in America today, and neither resolve the true crisis that the US faces, which is dealing with the disaster caused by the lockdown. Rather than insisting on staying at home, the left should argue for implementing an end to the lockdown that actually answers the demands of the workers striking at Amazon, Checkers, Instacart, and elsewhere for safe working conditions and worker’s rights.
A recent bill proposed by senators Sanders, Harris and Markey – which includes expanded unemployment insurance and the waiving of all student loan payments during the crisis – is a good start. But more must be done to address the structural inequalities that have made the coronavirus so deadly in the first place.
Universal healthcare and a complete overhaul of working conditions and unemployment benefits must be part of any comprehensive strategy for economic recovery. So is a massive public investment program that doesn’t just focus on propping up the stock market, but actually creates long-lasting and well-paid jobs.
The objections that were routinely raised against such proposals before the Covid-19 emergency centered on the difficulty of financing such programs. But if the way we have responded to the crisis has taught us anything, it’s that the money can be found when there’s a political will for it. It’s just a question of who we want it to benefit.
By : Joshua Craze and Carlo Invernizzi-Accetti
Date : May 16, 2020
Source : The Guardian
https://www.theguardian.com/commentisfree/2020/may/16/covid-19-coronavirus-lockdown-economy-debate
Not all kids have computers – and they’re being left behind with schools closed by the coronavirus
The big idea
Since 2014, the Dornsife Center for Economic and Social Research, located at the University of Southern California, has been tracking trends in health economic well-being, attitudes and behaviors through a nationwide survey for its Understanding America Study, asking the same individuals questions over time.
The nationally representative survey is now assessing how COVID-19 is affecting U.S. families. This includes their health, economic status and, for the first time, educational experiences. With two other education researchers Amie Rapaport and Marshall Garland, we analyzed the educational experience data that have recently been added to the study.
What we did
We worked with the broader Understanding America Study team to ask Americans about the effects the pandemic is having on students and their families.
About 1,450 families with children answered these questions between April 1 and April 15.
We found that nearly all – about 85% – of families with at least one child between kindergarten and their senior year of high school have internet access and a computer they can use for distance learning while school buildings are shuttered.
However, we found large disparities in technology access based on family income. Among the 20% of American households who make US$25,000 or less a year, just 63% of schoolchildren have access to a computer and the internet. In comparison, essentially all students from the most affluent families – those whose parents make $150,000 annually or more – do.
To be sure, that doesn’t mean a third of poor kids are being locked out of getting an online education. Many of those students are also using tablets and smartphones to participate in educational activities. However, the types of educational activities a student can easily engage in with a computer and wireless internet –such as writing long essays – are broader than the types possible on a tablet or an even smaller screen and with just a cellular connection.
These inequities can leave low-income families scrambling for wireless access. Some of the limited options available can include include working from a car parked outside a local library or a McDonald’s parking lot.
Why it matters
There’s a big gap between how much access rich and poor children have to technology. This is known as the “digital divide.”
This disparity contributes to the achievement gaps between students based largely on their economic status.
These findings show that the digital divide is playing out in real time during this pandemic in ways that are sure to lead to unequal negative effects on already disadvantaged students.
What’s next?
Most schools in the country are likely to remain closed for months – long after we collected this initial data. We believe that it’s possible that this divide will narrow once more districts distribute computers, tablets and other hardware, more communities take steps to expand broadband access to those who can’t afford it and teachers get better at educating kids online.
There’s a chance that federal help could arrive, should Congress pass the Emergency Educational Connections Act of 2020, a measure authored and backed by House Democrats aimed at narrowing the digital divide. It would normally be states – which provide the largest share of funding for public schools – that would address issues like technology in schools, but with states facing mounting budget constraints that’s going to be a big challenge. A similar bill is pending in the Senate.
In our view, without federal intervention, these gaps will not meaningfully narrow.
By : Morgan Polikoff (Associate Professor of Education, University of Southern California)
Anna Rosefsky Saavedra (Research Scientist, University of Southern California – Dornsife College of Letters, Arts and
Sciences)
Shira Korn (PhD Student K-12 Education Policy, University of Southern California)
Date : May 8, 2020
Source : The Conversation
https://theconversation.com/not-all-kids-have-computers-and-theyre-being-left-behind-with-schools-closed-by-the-coronavirus-137359
Counting the human cost of Covid-19: 'Numbers tell a story words can't'
The Guardian’s data journalists in the UK, US and Australia explain how they have shone a light on the statistical narrative behind the pandemic, and what they have helped to reveal
Mona Chalabi, data editor, Guardian US
Creating data journalism about Covid-19 has felt different. For one thing, the public aren’t thinking of the statistics as dry and abstract: they understand how critical they are. People are learning about methodologies and bell curves and logarithmic scales because they’re no longer inclined to look away from the screen when they see those words. That means there are also huge opportunities to learn and for people to change their (usually negative!) relationship with numbers.
I think we’ve always had the responsibility to inform without making people feel afraid, alone or sad. At first though, especially here in the US, it felt like not enough people were sufficiently scared. It was fear that was compelling me to stay at home – fear of making other people sick and fear of getting sick myself. So I was trying to create data visualisations that had that emotional resonance too. Illustrations that showed the numbers in a way that communicated the seriousness of this situation. I think that now the need has shifted a little where most people grasp the gravity of the situation. They need information about how to cope.
Caelainn Barr, data projects editor
Data is key in this crisis. It tells us the story of how the virus is spreading, who it affects most and, with political will, it could help pave the way out.
I am fascinated by what is left out of datasets. What we collect and omit tells us something about what we value and overlook as a society. If you don’t have data you can’t understand a problem or begin to formulate effective public policy to address it. As a journalist the gaps in datasets also give you a sense of what is not understood and should be examined in greater depth. This line of thinking has informed much of our reporting to date.
We have uncovered flaws in the government death toll, shown how the most deprived would be disproportionately affected if parks were closed, revealed BAME people are more at risk of dying from Covid-19, and explored why the poor are twice as likely to die of the virus as the rich.
Work is incredibly demanding at the moment. Very often we’re trying to make sense of new information and patchy datasets in a rapidly evolving crisis. So far data has shown us that the virus is certainly not a social leveller, rather it has found the cracks in society and blown them wide open, making long-standing inequalities painfully clear. By inquiring beyond the headline numbers, data can help us understand who the virus is affecting the most so we can forge a fairer society once this has passed.
Pamela Duncan, data journalist
Counting the human cost of the coronavirus has been one of the greatest challenges faced professionally by journalists since the onset of the pandemic: even the number of deaths is genuinely hard to provide.
Part of the problem is that data collection and reporting by the responsible agencies in the UK and elsewhere has been slow to become uniform: ordinarily deaths are collected by statistical bodies with a delay. But deaths due to Covid-19 are of obvious public interest and so the figures need to be circulated. Therefore, for data journalists like myself, much of the past two months has been spent chasing data; figuring out which deaths have and have not been included in various organisations’ figures; finding out what we can and cannot compare.
As a Guardian journalist you are always focused on reporting the truth. Never has this been more pronounced than in this crisis, where you are hyper-aware that underreporting the figures could cause complacency whereas exaggerating them could cause panic. Some have criticised journalists for not being critical enough while others wrongly, and dangerously, suggest that the figures are exaggerated. But it isn’t those people we concern ourselves with: it is getting to the truth and pointing out what we know when we know it. This means that we aren’t just putting out a BIG FIGURE and leaving it at that. Instead we are explaining why we think the BIG FIGURE isn’t the whole picture. We have faith in our audience’s ability to recognise that we may not have all the answers right now but that we are working tirelessly to get them.
Nick Evershed, data and interactives editor, Guardian Australia
Australia is now a success story in terms of its early response to Covid-19, with new cases now often below 20 a day, and far fewer deaths per million people than other countries. How this early success in flattening the curve transitions into an easing of restrictions and the prospect of a second wave remains to be seen.
When the pandemic started worsening in Australia, there were significant challenges with reporting on basic aspects of the outbreak.
Because of the difference in reporting times and methods, getting basic information correct such as the number of cases, deaths, and testing rates required staying on top of information released by nine governments.
Inspired by other projects doing similar work we started tracking these figures internally, and then decided to release the data with a licence allowing reuse. This decision paid off – the data has been used by researchers, private companies and ordinary citizens to analyse and visualise the pandemic’s impact on Australia.
Having the data openly accessible also means our figures are constantly being checked, ensuring they are as accurate as possible. This was especially helpful in the early days when significant time pressure would inevitably mean some mistakes – thankfully quickly corrected in response to reader emails.
The response has been phenomenal. The summary page has been one of the most popular pieces we have produced during the pandemic, with 5.4m page views at the time of writing. The data also is used in all our liveblogs to give readers a quick summary of the current situation.
Niko Kommenda, visual projects editor, and Pablo Gutiérrez, visual artist
We realised very early on that the story of the coronavirus crisis would benefit hugely from visually led coverage – we published our first visual explainer on the topic in early February, when the overwhelming majority of confirmed cases and deaths were still being reported in China.
From this early stage, our audience was eager to understand the details of the story. We wanted to report on it in a way that was easy to understand and offered clear conclusions. Using maps and charts, we were able to analyse the quantity and speed with which the disease multiplied each day. Our visual trackers evolved as we were able to establish comparisons between countries, put the data into historical context and shed light on different scenarios playing out in different regions.
Visual journalists around the world are coming up with ever more ingenious ways of explaining and contextualising the numbers, from case counts to reproduction numbers, to the tragic death toll of the virus.
“Flatten the curve” is perhaps the best example of a visualisation so well designed and so memorable that it has become a universally understood metaphor for a concept that would require a much lengthier explanation if one tried to convey it through words alone.
Our team is following the lively debate within the data visualisation community closely, and we’re constantly working to improve our own coronavirus trackers while experimenting with new formats to communicate the scale of the emergency. We have also experienced a growing interest from our readers in how we make our graphics, with a variety of questions reaching us each day via email and social networks.
As the global pandemic continues, we’re using visuals to drive home the dramatic change that the virus has spurred in the way we live and work – from mapping how lockdown measures have slashed global air pollution to quantifying the disastrous impact on the economy.
Source : The Guardian
https://www.theguardian.com/membership/datablog/2020/may/09/data-covid-19-numbers-story-pandemic-guardian-statistics
Which Covid-19 Data Can You Trust?
The Covid-19 pandemic has created a tidal wave of data. As countries and cities struggle to grab hold of the scope and scale of the problem, tech corporations and data aggregators have stepped up, filling the gap with dashboards scoring social distancing based on location data from mobile phone apps and cell towers, contact-tracing apps using geolocation services and Bluetooth, and modeling efforts to predict epidemic burden and hospital needs. In the face of uncertainty, these data can provide comfort — tangible facts in the face of many unknowns.
In a crisis situation like the one we are in, data can be an essential tool for crafting responses, allocating resources, measuring the effectiveness of interventions, such as social distancing, and telling us when we might reopen economies. However, incomplete or incorrect data can also muddy the waters, obscuring important nuances within communities, ignoring important factors such as socioeconomic realities, and creating false senses of panic or safety, not to mention other harms such as needlessly exposing private information. Right now, bad data could produce serious missteps with consequences for millions.
Unfortunately, many of these technological solutions — however well intended — do not provide the clear picture they purport to. In many cases, there is insufficient engagement with subject-matter experts, such as epidemiologists who specialize in modeling the spread of infectious diseases or front-line clinicians who can help prioritize needs. But because technology and telecom companies have greater access to mobile device data, enormous financial resources, and larger teams of data scientists, than academic researchers do, their data products are being rolled out at a higher volume than high quality studies.
Whether you’re a CEO, a consultant, a policymaker, or just someone who is trying to make sense of what’s going on, it’s essential to be able to sort the good data from the misleading — or even misguided.
Common Pitfalls
While you may not be qualified to evaluate the particulars of every dashboard, chart, and study you see, there are common red flags to let you know data might not be reliable. Here’s what to look out for:
Data products that are too broad, too specific, or lack context. Over-aggregated data — such as national metrics of physical distancing that some of our largest data aggregators in the world are putting out — obscure important local and regional variation, are not actionable, and mean little if used for inter-nation comparisons given the massive social, demographic, and economic disparities in the world.
Conversely, overly disaggregated data can do outright harm. Public health practitioners and data privacy experts rely on proportionality — only use the data that you absolutely need for the intended purpose and no more. To some extent, all data risk breaching the privacy of individual or group identities, but publishing scorecards for specific neighborhoods risks shaming or punishing communities, while ignoring the socioeconomic realities of people’s lives that make it difficult for them to stay home. Even more granular examples, such as footfalls at identifiable business locations, risks de-identifying religious groups; patients visiting cancer hospitals, HIV clinics, or reproductive health clinics; or those seeking public assistance. The medical and public health communities long ago deemed the un-masking of such information without consent unacceptable, but companies have recently been releasing it on publicly available dashboards.
Even data at an appropriate spatial resolution must be interpreted with caution — context is key. Say you see a map that shows a 20% decrease in mobility in an American suburb and a 40% decrease in a nearby city after social distancing measures are announced. The decrease in the suburb may adequately push physical distancing to below the desired threshold, given that its residents started with a relatively low baseline to begin with. The city may still be far away from the mobility reduction required to meaningfully impact transmission rates, as its residents were very mobile before. Until we know more about how these changing movement patterns impact epidemiological aspects of the disease, we should use these data with caution. Simply presenting them, or interpreting them without a proper contextual understanding, could inadvertently lead to imposing or relaxing restrictions on lives and livelihoods, based on incomplete information.
The technologies behind the data are unvetted or have limited utility. Tech solutions such as mobile phone-based contact tracing — a solution gaining steam in many countries — have untested potential, but only as part of a broader comprehensive strategy that includes a strong underlying health system. Jason Bay, the product lead of Singapore’s successful tracing app, TraceTogether, cautions that “automated contact tracing is not a coronavirus panacea.” Yet some app-based contact-tracing efforts are being used to risk-stratify people, and these estimates are being used to make decisions on quarantine, isolation, and freedom of movement, without concomitant testing.
Both producers and consumers of outputs from these apps must understand where these can fall short. They may prove to be very useful if we experience recurrent waves in the coming months, when the outbreaks may be more localized, and our testing capacity commensurate with our technological aspirations. In the absence of a tightly coupled testing and treatment plan, however, these apps risk either providing false reassurance to communities where infectious but asymptomatic individuals can continue to spread disease, or requiring an unreasonably large number of people to quarantine. The behavioral response of the population to these apps is therefore unknown and likely to vary significantly across societies.
In some cases, the data from tracing apps requires another caveat: the methods they use are not transparent, so they cannot be fully evaluated by experts. Some contact-tracing apps follow black-box algorithms, which preclude the global community of scientists from refining them or adopting them elsewhere. These non-transparent, un-validated interventions — which are now being rolled out (or rolled back) in countries such as China, India, Israel and Vietnam — are in direct contravention to the open cross-border collaboration that scientists have adopted to address the Covid-19 pandemic. Only transparent, thoroughly vetted algorithms should be considered to augment public health interventions that affect the lives of millions.
Models are produced and presented without appropriate expertise. Well-meaning technologists and highly influential consulting firms are advising governments, and consequently businesses and general populations around the world, on strategies to combat the epidemic, including by building projection and prediction models. Epidemiological models that can help predict the burden and pattern of spread of Covid-19 rely on a number of parameters that are, as yet, wildly uncertain. We still lack many of the basic facts about this disease, including how many people have symptoms, whether people who have been infected are immune to reinfection, and — crucially — how many people have been infected so far. In the absence of reliable virological testing data, we cannot fit models accurately, or know confidently what the future of this epidemic will look like for all these reasons, and yet numbers are being presented to governments and the public with the appearance of certainty
Take a recent example: A leading global consulting firm explained their projections for an east-coast American city, by overlaying on it what they referred to as “the Wuhan curve.” The two populations and cities could not be more different in their demography and health care infrastructure. Such oversimplifications risk inaccurate projections and the untimely diversion of critical resources from places that need them the most. Corporations have the vast resources required to rapidly translate the knowledge generated from their data and technologies to governments and communities, but are crowdsourcing expertise from within their ranks. While it can be tempting to want to move with speed, a rapid “move fast and break things” approach — the hallmark of our startup culture — is inappropriate here. Coupling this enthusiasm with the right kind of subject matter expertise may go farther.
Read Carefully and Trust Cautiously
Relying on trustworthy sources is always good advice, but now it is an absolute must. Here are some buoys to help you navigate your way to the shore, whether you are a producer or consumer of data.
Transparency: Look for how the data, technology, or recommendations are presented. The more transparent the providers are about the representativeness of their data, analytic methods, or algorithms, the more confident they are of their process, and more open to public scrutiny. These are the safest knowledge partners.
Example: Singapore’s government was entirely transparent about the code, algorithm, and logic used in its TraceTogether contact app. While launching the app, they openly published a policy brief and white paper describing the rational and working of the app, and most importantly, their protocol (“BlueTrace”) and codebase (“OpenTrace”), allowing open review.
Thoughtfulness: Look for signs of hubris. Wanton disregard of privacy, civil rights, or well-established scientific facts belie overconfidence at best, and recklessness at worst. These kinds of approaches are likely to result in the most harm. Analysts that are conservative in their recommendations, share the uncertainty associated with their interpretations, and situate their findings in the appropriate local context are likely to be more useful.
Example: Telenor, the Norwegian telco giant has led the way in responsible use of aggregated mobility data from cell phone tower records. Its data have been used, in close collaboration with scientists and local practitioners, to model, predict, and respond to outbreaks around the world. Telenor has openly published its methods and provided technological guidance on how telco data can be used in public health emergencies in a responsible, anonymized format that does not risk de-identification.
Expertise: Look for the professionals. Examine the credentials of those providing and processing the data. We are facing a deluge of data and interpretation from the wrong kinds of experts, resulting in a high noise-to-signal ratio. On the most bullish of days, we wouldn’t want our bankers to be our surgeons.
Example: Imperial College, among other academic groups, has been involved in guiding decision makers in the U.K. Covid-19 response since the early days of the epidemic, through the work of the MRC Center for Global Infectious Disease Analysis. In the U.S., longstanding collaborations between state and local health departments and research groups have been augmented by new collaborative partnerships. In both countries, these efforts critically rely on sustained funding of centers that can support methods development and training during inter-epidemic periods and mobilized to respond when crises hit.
Open Platforms: Look for the collaborators. There are several data aggregators that are committed to supporting an ecosystem of communities, businesses, and research partners, by sharing data or code in safe and responsible ways. Such open ecosystem approaches, while not easy to manage, can yield high dividends.
Example: Where technology companies like Camber Systems, Cubeiq and Facebook have allowed scientists to examine their data, researchers can compare data across these novel data streams to account for representativeness and correct biases, making the data even more useful. The Covid-19 Mobility Data Network, of which we are part, comprises a voluntary collaboration of epidemiologists from around the world analyzes aggregated data from technology companies to provide daily insights to city and state officials from California to Dhaka, Bangladesh. Governments convey what information gaps exist in their planning and policy making, the scientists help identify the best analytic approaches to address those gaps, and the technology companies make available the data they have access to in a meaningful, interpretable format. All data exchange follows strict institutional ethical guidelines and is in compliance with local and international law. Daily outputs speak to the articulated needs of the collaborating government officials.
This pandemic has been studied more intensely in a shorter amount of time than any other human event. Our globalized world has rapidly generated and shared a vast amount of information about it. It is inevitable that there will be bad as well as good data in that mix. These massive, decentralized, and crowd-sourced data can reliably be converted to life-saving knowledge if tempered by expertise, transparency, rigor, and collaboration. When making your own decisions, read closely, trust carefully, and when in doubt, look to the experts.
By : Satchit Balsari, Caroline Buckee and Tarun Khanna
Date : May 08, 2020
Source: Harvard Business Review (https://hbr.org/2020/05/which-covid-19-data-can-you-trust?ab=hero-main-text)
Why are more men dying from COVID-19?
The novel coronavirus tends to affect men more severely than it does women. Though nobody can yet explain the oddity, researchers are hot on the case.
It's possible that the sex hormones estrogen and testosterone play a role, according to previous research on respiratory illnesses. Or perhaps it's because the X chromosome (which women have two of, but men have only one) has a larger number of immune-related genes, giving women a more robust immune system to fight off the coronavirus, SARS-CoV-2. Or, maybe the virus is hiding in the testes, which has abundant expression of ACE2 receptors, the portal that allows SARS-CoV-2 into cells.
Uncovering the real reason is, of course, imperative because it could help improve patient "outcomes during an active public health crisis," according to an editorial published April 10 in the Western Journal of Emergency Medicine (WJEM).
What are the numbers?
Since the first known COVID-19 case was reported in China late last year, countless studies have shown that the disease tends to be more severe and deadly in men than in women.
For instance, in an analysis of 5,700 COVID-19 patients hospitalized in New York City, just over 60% were men, according to an April 22 study published in the journal JAMA. What's more, "mortality rates were higher for male compared with female patients at every 10-year age interval older than 20 years," the researchers wrote in the study.
Furthermore, of the 373 patients who ended up in intensive care units, 66.5% were men, the JAMA study reported.
Results are similar in other studies. When the WJEM editorial was published in early April, the authors noted that between 51% and 66.7% of hospitalized patients in Wuhan, China, were male; 58% in Italy were male; and 70% of all COVID-related deaths worldwide were male. In one large study of more than 44,600 people with COVID-19 in China, 2.8% of men died versus just 1.7% of women.
Are men more susceptible?
These COVID-19 sex differences are not unexpected. Other coronavirus outbreaks, including outbreaks of SARS in 2003 and the Middle East respiratory syndrome (MERS) in 2012, had higher fatality rates in men than in women, according to the WJEM editorial. For example, a 2016 study found that men had a 40 percent higher odds of dying of MERS than women did.
Even the comically labeled "man flu" is so named because men tend to have a weaker immune response to respiratory viruses that cause flu and the common cold. As a result, men tend to get more severe symptoms from these viruses than women do, a 2017 review in BMJ found. That review pinned these results on the differences in "sex dependent hormones" in men and women.
A mouse experiment offers clues about this hormonal mystery; when scientists infected both male and female mice of different ages with SARS, the male mice were more susceptible to the infection than females of the same age, according to a 2017 study, which was published in The Journal of Immunology. However, when the female mice had their estrogen-producing ovaries removed or were treated with an estrogen-receptor blocker, they died at higher rates than those with working ovaries and normal estrogen.
"These data indicate that sex hormones produced in female [mice] may help to defend against coronaviruses like SARS and SARS-CoV-2," Akiko Iwasaki, a professor of immunobiology at Yale University School of Medicine, who was not involved in the study, told Live Science.
To learn more, scientists at Cedars-Sinai Medical Center in Los Angeles and the Renaissance School of Medicine at Stony Brook University in New York are testing estrogen or another sex hormone called progesterone on small groups of people who have COVID-19, Live Science previously reported.
There's another way to look at the COVID-19 sex difference; perhaps the X chromosome is protective because it has more immune-related genes than the Y chromosome does. This may also explain why women are more likely than men to have autoimmune diseases, the authors of the WJEM editorial noted.
The second X chromosome is usually silenced in women, but almost 10% of those genes can be activated, Veena Taneja, who studies differences in male and female immune systems at the Mayo Clinic, told NPR. "Many of those genes are actually immune-response genes," she said. This could give women a "double-dose" of protection, Taneja said, although research is needed to see whether these genes factor into protection against COVID-19.
Hiding in the testes?
New research offers yet another idea; men seem to clear SARS-CoV-2 from their bodies more slowly than women do. To explain that possibility, researchers have suggested the virus may have found a hiding place in men: the testes.
In the research, published on the preprint medRxiv database, 68 people confirmed to have COVID-19 in Mumbai, India, were tested with nasal swabs until they tested negative for the virus. At the end of the experiment, scientists found that women cleared the virus from their bodies in an average of 4 days, compared with men's average of 6 days. The same test in three different Mumbai households found similar results.
"Our collaborative study found that men have more difficulty clearing coronavirus following infection, which could explain their more serious problems with COVID-19 disease," study lead researcher Dr. Aditi Shastri, assistant professor of medicine at the Albert Einstein College of Medicine in New York City and a clinical oncologist at the Montefiore Einstein Center for Cancer Care, said in a statement.
Previous research has shown that SARS-CoV-2 invades certain human cells by plugging into these cells' ACE2 receptors. So, the researchers consulted a database, and found that the testes have high levels of ACE2 expression. In contrast, ACE2 could not be detected in the ovaries, the female equivalent of the testes.
However, the research did not actually look in the testes to see if SARS-CoV-2 is hanging out there, so "it does not tell us whether the virus infects testes or whether it is a reservoir of virus," said Iwasaki, who was not involved in the research.
What about smoking?
Other research has suggested that smoking may play a role, as smoking is related to higher expression of ACE2 receptors. But while more men than women smoke in China, that's not true in other countries, which likely puts a kibosh on smoking to explain the sex difference.
"What we saw in Wuhan [with the sex difference] has been replicated in every country around the world where we have accurate reporting," Sabra Klein, a researcher at the Johns Hopkins Center for Women's Health, Sex, and Gender Differences, told NPR. "In countries like Spain, where the percentages of males and females who report smoking is not significantly different, we still are seeing this profound male bias in severity of COVID-19."
Other explanations: Women are simply less likely to engage in health-related risks and are better at washing their hands, studies find, and perhaps that's behind the gender disparity
Sex differences aren't the only factor at play, however. Other groups more vulnerable to COVID-19 include the elderly and people with diabetes, high blood pressure and obesity, Live Science previously reported.
- 20 of the worst epidemics and pandemics in history
- 28 Devastating Infectious Diseases
- 11 Surprising Facts About the Respiratory System
By : Laura Geggel - Associate Editor
Date : April 28, 2020
Source : Live Science
https://www.livescience.com/why-covid-19-more-severe-men.html
How the COVID-19 lockdown will take its own toll on health
NEW YORK (Reuters) - It’s the most dramatic government intervention into our lives since World War II. To fight the coronavirus outbreak, governments across the globe have closed schools, travel and businesses big and small. Many observers have fretted about the economic costs of throwing millions of people out of work and millions of students out of school.
Now, three weeks after the United States and other countries took sweeping suppression steps that could last months or more, some public health specialists are exploring a different consequence of the mass shutdown: the thousands of deaths likely to arise unrelated to the disease itself.
The longer the suppression lasts, history shows, the worse such outcomes will be. A surge of unemployment in 1982 cut the life spans of Americans by a collective two to three million years, researchers found. During the last recession, from 2007-2009, the bleak job market helped spike suicide rates in the United States and Europe, claiming the lives of 10,000 more people than prior to the downturn. This time, such effects could be even deeper in the weeks, months and years ahead if, as many business and political leaders are warning, the economy crashes and unemployment skyrockets to historic levels.
Already, there are reports that isolation measures are triggering more domestic violence in some areas. Prolonged school closings are preventing special needs children from receiving treatment and could presage a rise in dropouts and delinquency. Public health centers will lose funding, causing a decline in their services and the health of their communities. A surge in unemployment to 20% – a forecast now common in Western economies – could cause an additional 20,000 suicides in Europe and the United States among those out of work or entering a near-empty job market.
None of this is to downplay the chilling death toll COVID-19 threatens, or to suggest governments shouldn’t aggressively respond to the crisis.
A recent report by researchers from Imperial College London helped set the global lockdown in motion, contending that coronavirus could kill 2 million Americans and 500,000 people in Great Britain unless governments rapidly deployed severe social distancing measures. To truly work, the report said, the suppression effort would need to last, perhaps in an on-again, off-again fashion, for up to 18 months.
In the United States, the White House this week said the final toll could rise to 240,000 dead. States have responded to the dire warnings, and the escalating number of cases revealed each day, by extending stay-at-home shutdowns.
The medical battle against COVID-19 is developing so rapidly that no one knows how it will play out or what the final casualty count will be. But researchers say history shows that responses to a deep and long economic shock, coupled with social distancing, will trigger health impacts of their own, over the short, mid and long term.
Here is a look at some.
SHORT TERM CONSEQUENCES
Domestic Violence
Trapped at home with their abusers, some domestic violence victims are already experiencing more frequent and extreme violence, said Katie Ray-Jones, the chief executive officer of the National Domestic Violence Hotline.
Domestic violence programs across the country have cited increases in calls for help, news accounts reported – from Cincinnati to Nashville, Portland, Salt Lake City and statewide in Virginia and Arizona. The YWCA of Northern New Jersey, in another example, told Reuters its domestic violence calls have risen up to 24%.
“There are special populations that are going to have impacts that go way beyond COVID-19,” said Ray-Jones, citing domestic violence victims as one.
Vulnerable Students
Students, parents and teachers all face challenges adjusting to remote learning, as schools nationwide have been closed and online learning has begun.
Some experts are concerned that students at home, especially those living in unstable environments or poverty, will miss more assignments. High school students who miss at least three days a month are seven times more likely to drop out before graduating and, as a result, live nine years less than their peers, according to a Robert Wood Johnson Foundation report.
Among the most vulnerable: the more than 6 million special education students across the United States. Without rigorous schooling and therapy, these students face a lifetime of challenges.
Special needs students “benefit the most from highly structured and customized special education,” said Sharon Vaughn, executive director of the The Meadows Center for Preventing Educational Risk at the University of Texas. “This means that they are the group that are most likely to be significantly impacted by not attending school both in the short and long term.”
In New Jersey, Matawan’s Megan Gutierrez has been overwhelmed with teaching and therapy duties for her two nonverbal autistic sons, eight and 10. She’s worried the boys, who normally work with a team of therapists and teachers, will regress. “For me, keeping those communications skills is huge, because if they don’t, that can lead to behavioral issues where they get frustrated because they can’t communicate,” Gutierrez said.
MEDIUM TERM CONSEQUENCES
Soaring Suicides
In Europe and the United States, suicide rates rise about 1% for every one percentage point increase in unemployment, according to research published by lead author Aaron Reeves from Oxford University. During the last recession, when the unemployment in the United States peaked at 10%, the suicide rate jumped, resulting in 4,750 more deaths. If the unemployment rate increases to 20%, the toll could well rise.
“Sadly, I think there is a good chance we could see twice as many suicides over the next 24 months than we saw during the early part of the last recession,” Reeves told Reuters. That would be about 20,000 additional dead by suicide in the United States and Europe.
Less than three weeks after extreme suppression measures began in the United States, unemployment claims rose by nearly 10 million. Treasury Secretary Steven Mnuchin warned the rate could reach 20% and Federal Reserve economists predicted as high as 32%. Europe faces similarly dire forecasts.
Some researchers caution that suicide rates might not spike so high. The conventional wisdom is that more people will kill themselves amid skyrocketing unemployment, but communities could rally around a national effort to defeat COVID-19 and the rates may not rise, said Anne Case, who researches health economics at Princeton University. “Suicide is hard to predict even in the absence of a crisis of Biblical proportions,” Case said.
This week, the Air Force Academy in Colorado Springs, Colorado, relaxed its strict social isolation policies after the apparent suicides of two cadet seniors in late March, The Gazette, a Colorado Springs newspaper, reported. While juniors, sophomores and freshmen had been sent home, the college seniors were kept isolated in dorms, and some had complained of a prison-like setting. Now, the seniors will be able to leave campus for drive-thru food and congregate in small groups per state guidelines.
Public Health Crippled
Local health departments run programs that treat chronic diseases such as diabetes. They also help prevent childhood lead poisoning and stem the spread of the flu, tuberculosis and rabies. A severe loss of property and sales tax revenue following a wave of business failures will likely cripple these health departments, said Adriane Casalotti, chief of government affairs with the National Association of County and City Health Officials, a nonprofit focused on public health.
After the 2008 recession, local health departments in the U.S. lost 23,000 positions as more than half experienced budget cuts. While it’s become popular to warn against placing economic concerns over health, Casalotti said that, on the front lines of public health, the two are inexorably linked. “What are you going to do when you have no tax base to pull from?” she asked.
Carol Moehrle, director of a public health department that serves five counties in northern Idaho, said her office lost about 40 of its 90 employees amid the last recession. The department had to cut a family planning program that provided birth control to women below the poverty line and a program that tested for and treated sexually transmitted diseases. She worries a depression will cause more harm.
“I honestly don’t think we could be much leaner and still be viable, which is a scary thing to think about,” Moehrle said.
LONG TERM CONSEQUENCES
Job-loss Mortality
Rises in unemployment during large recessions can set in motion a domino effect of reduced income, additional stress and unhealthy lifestyles. Those setbacks in income and health often mean people die earlier, said Till von Wachter, a University of California Los Angeles professor who researches the impact of job loss. Von Wachter said his research of past surges in unemployment suggests displaced workers could lose, on average, a year and a half of lifespan. If the jobless rate rises to 20%, this could translate into 48 million years of lost human life.
Von Wachter cites measures he believes could mitigate the effects of unemployment. The Coronavirus Aid, Relief, and Economic Security Act approved by the White House last week includes emergency loans to businesses and a short-time compensation program that could encourage employers to keep employees on the payroll.
Young People Suffer
Young adults entering the job market during the coronavirus suppression may pay an especially high price over the long term.
First-time job hunters seeking work during periods of high unemployment live shorter and unhealthier lives, research shows. An extended freeze of the economy could shorten the lifespan of 6.4 million Americans entering the job market by an average of about two years, said Hannes Schwandt, a health economics researcher at Northwestern University, who conducted the study with von Wachter. This would be 12.8 million years of life lost.
Thousands of college graduates will enter a job market at a time global business is frozen. Jason Gustave, a senior at William Paterson University in New Jersey who will be the first in his family to graduate from college, had a job in physical therapy lined up. Now his licensure exam is postponed and the earliest he could start work is September.
“It all depends on where the economy goes,” he said. “Is there a position still available?”
WHAT COMES NEXT
In the weeks ahead, a clearer picture of the disease’s devastation will come into focus, and governments and health specialists will base their fatality estimates on a stronger factual grounding.
As they do, some public health experts say, the government should weigh the costs of the suppression measures taken and consider recalibrating, if necessary.
Dr. Jay Bhattacharya, who researches health policy at Stanford University, said he worries governments worldwide have not yet fully considered the long term health impacts of the impending economic calamity. The coronavirus can kill, he said, but a global depression will, as well. Bhattacharya is among those urging government leaders to carefully consider the complete shutdown of businesses and schools.
“Depressions are deadly for people, poor people especially,” he said.
Reporting in New York by M.B. Pell and Benjamin Lesser. Data editing by Janet Roberts. Editing by Ronnie Greene.
Date : April 3, 2020
Source : Reuters
https://uk.reuters.com/article/uk-health-coronavirus-usa-cost-special-r/special-report-how-the-covid-19-lockdown-will-take-its-own-toll-on-health-idUKKBN21L21K
Antarctic endeavours, primary health-care research and dark matter exploration – the coronavirus casualties you haven’t heard of
The year 2020 came with big expectations for researchers, myself included. Last year I was successful in the first round of the National Health and Medical Research Council Investigator Grants scheme. Six years since completing my PhD, I managed to launch my Healthy Primary Care research team.
We investigate how principles of wellness such as healthy eating and exercise are incorporated into health care, particularly in general practice. I spent the summer planning how to support my team for the next five years, focusing on impact and research translation into real-world settings.
Big things were in the works. It was an exciting time. But as it turns out, wellness in health care isn’t a priority during the COVID-19 crisis.
As the pandemic lingers, big players (especially pharmaceutical companies) around the world have understandably dropped everything, joining forces to give the virus their undivided attention.
A sudden loss
Many of my team’s projects relied on doctors, nurses and other health professionals to collect or provide data. With the strain placed on health care by the pandemic, continuing was no longer viable. Grant applications, domestic and international travel, conferences and meetings have all been cancelled or postponed indefinitely.
As a supervisor, the hardest part was withdrawing research students and interns I’d lined up to start projects in clinics. This pandemic has challenged the relevance, impact and productivity of our work.
This shock comes shortly after a summer of devastating bushfires which hindered research progress by forcing experts out of fire-affected regions, destroying expanses of equipment and reportedly setting some studies “back months or years”.
Stoppages across the field
Social distancing, travel bans and quarantine restrictions mean scientific fieldwork across the world has almost completely stopped.
The Australian Antarctic Program, led by the federal Department of Agriculture, Water and the Environment has been reduced to essential staff only to keep the Antarctic continent COVID-19-free. Instead of sending 500 expeditioners in the next summer season, the Australian Antarctic Division will only send about 150.
Social distancing measures are also preventing climate scientists from being able to visit their laboratories. If the pandemic continues, this could hamper important weather and climate surveillance practices. In some cases, labs have been reduced to one essential worker whose sole job is to keep laboratory animals alive for when research resumes.
Delays have also impacted one of the world’s largest efforts to investigate the nature of dark matter. The XENON experiment based in Italy is worth more than US$30 million, according to the New York Times. It faced a multitude of roadblocks when the country was forced into lockdown earlier this year.
Young research stars missing opportunities
For young researchers, social distancing and event cancellations are especially damaging to professional development. Scientific conferences and meetings foster collaboration and can also lead to employment opportunities.
This crisis has left the next generation of researchers unsupported, and have negative flow-on effects for all research areas. In health and disease prevention, research efforts apart from vaccinations are still vital, as the onset of COVID-19 hasn’t stopped the rise of chronic disease.
There are positives
Australia boasts a robust and passionate research workforce, which means we can divert resources to a united cause such as the coronavirus crisis. As the race for a vaccine continues, the value of research has never been more apparent to the non-scientific community. This may help weaken anti-science messages.
The pandemic is also providing opportunity for future university leaders to understand university management, funding and governance decisions. Never before has information been so accessible on where funding comes from.
Online conferencing and collaboration related to research has also made participation more accessible and affordable. This increases inclusively by removing barriers for people who may not be able to attend in-person gatherings, such as people living with a physical disability, full-time carers and people experiencing financial hardship. Less domestic and international travel is also helping reduce carbon footprints.
Charging forward
The health system isn’t working normally, which means my team’s research isn’t working normally. Nonetheless, we’re pivoting well in this uncertain time. We’re helping plan the first online conference for Australian primary care to improve access to relevant research across the country.
New grant opportunities are aligning COVID-19 to our research focus, such as the Royal Australian College of General Practitioners’s and the Hospitals Contribution Fund’s special call for projects on COVID-19 in general practice.
Some may think non-COVID-19 research isn’t currently necessary, but it will be once we combat this disease. And when that happens, we’ll be ready to right where we left off.
By : Lauren Ball (Associate Professor/ Principal Research Fellow, Griffith University)
Date : April 21, 2020
Source : The Conversation
https://theconversation.com/antarctic-endeavours-primary-health-care-research-and-dark-matter-exploration-the-coronavirus-casualties-you-havent-heard-of-136390
The Scariest Pandemic Timeline
If the flu and coronavirus hit at the same time this fall, America might have a longer, more severe lockdown.
If you held out a glimmer of hope about life returning to normal this year, that hope may have been thoroughly extinguished this week by the director of the Centers for Disease Control and Prevention, Robert Redfield.
“There’s a possibility that the assault of the virus on our nation next winter will actually be even more difficult than the one we just went through,” Redfield told The Washington Post on Tuesday. “We’re going to have the flu epidemic and the coronavirus epidemic at the same time.”
President Trump later tried to claim that Redfield had been misquoted, but Redfield clarified that he was quoted accurately. He’s also far from the only person who believes that the United States is in for a bleak winter. Numerous public-health experts are concerned that COVID-19 might make a comeback this fall (assuming that total case numbers even drop to begin with). In combination with the normal, October-through-March flu season, the disease could strain hospital capacity even more than it did this spring, when flu season was petering out. “It’s going to be a very difficult fall and winter this year coming up,” says Ashish Jha, the director of the Harvard Global Health Institute.
Scientists don’t yet know if the coronavirus will fade away during the summer before making a resurgence in colder temperatures. Some other respiratory illnesses do this: During the 2009 swine-flu outbreak, cases surged in the spring, subsided over the summer, then returned with a vengeance in the autumn. But the new coronavirus strain’s behavior is still too mysterious to predict for certain. Experts expect the virus to circulate among humans for some time, but its particular ebbs and flows aren’t yet known.
A late-in-the-year rebound would be a problem because flu season already puts hospitals close to capacity, experts told me. Though fewer people hospitalized for the flu would require ventilators than COVID-19 patients likely would, flu patients might need precious intensive-care-unit space. Already during this outbreak, reports from hospitals read like dispatches from a war zone. One 49-year-old COVID-19 patient was found “blue and dead” in an emergency-room chair while waiting for an inpatient bed. Doctors’ groups debated whether younger patients should have preferential access to ventilators. Having to contend with another round of COVID-19 patients while also taking on severe flu cases might cause hospitals to quickly run out of ventilators, beds, or even doctors.
Some people might even get infected with both the flu and COVID-19 at the same time. While health experts don’t know exactly how that would make COVID-19 worse, “I can’t imagine that would be good,” Jennifer Nuzzo, a senior scholar at the Johns Hopkins Center for Health Security, said.
Even as the seasonal flu reenters the picture, Americans likely won’t have developed herd immunity to COVID-19, and a vaccine is likely still more than a year away. The absolute safest thing to do would be for all Americans to lock themselves inside until there’s a coronavirus vaccine. However, even die-hard public-health cheerleaders say that’s simply not feasible. Millions of people have lost their jobs; non-COVID-19 medical treatments are being postponed; children are suffering from a lack of schooling and socialization.
Instead, health experts broadly concur that the best path forward will be an aggressive testing and contact-tracing regimen. It might not be possible to get asymptomatic people tested regularly. However, the rapid testing of anyone who has possible COVID-19 symptoms, along with a way to track and isolate anyone they’ve been in contact with, could keep coronavirus infections from spreading as the flu simultaneously rips through the population. While America’s testing capabilities have been increasing, we are currently not testing or contact-tracing at anywhere near the necessary level, experts say.
There are other ways to prepare for a big fall surge in flu and COVID-19 infections. Government and hospital officials could use the intervening time to staff up hospitals and increase their capacity. Large sporting events and concerts may need to be postponed until there’s more immunity in the population, Nuzzo and others say. Jha says universities should cancel sports and extracurriculars, give every student a single dorm, and stagger dining times. Vulnerable people—like the elderly or those with chronic illnesses—may have to stay home longer than others. Everyone could wear masks even after they’re no longer required to, and work from home if they’re able to.
In addition to mitigating coronavirus transmission, these types of mild social-distancing measures might help reduce the spread of the flu. “Some of these things will hopefully work their way into our more normal, day-to-day lives, and we’ll be able to do ‘social distancing light’ in a way that will help us reduce the transmission,” Stephen Kissler, an infectious-disease modeler at Harvard, told me.
Jha is hopeful that between now and this fall, biotech companies will have developed drugs that can lessen COVID-19 symptoms. Though these might not be “cures” per se, they might reduce the amount of time COVID-19 patients are in the hospital and thus ease the strain on the health-care system. If these measures don’t happen, Americans might see additional lockdowns. “If we don’t get our act together, the chances that there will be another lockdown in the fall, and that it will be a long one, are very, very high,” Jha said.
To be sure, even if no one takes unnecessary risks, and therapeutics are available, and the hospitals are well stocked, and hand-washing becomes a religion, there still might need to be a fall lockdown. This is, unfortunately, the new uncertainty with which we all now live.
If you are desperate to cling to some modicum of control, the number-one way everyday Americans can help to prevent this flu-COVID-19 Armageddon is by getting the flu shot. Employers could even make returning to work in the fall contingent on being vaccinated against the flu, Nuzzo said. The flu shot is one of the few things that are within our power, and it doesn’t rely on the vicissitudes of pathogens. There aren’t many opportunities to feel empowered these days. We might want to seize the ones we get.
OLGA KHAZAN is a staff writer at The Atlantic and the author of Weird: The Power of Being an Outsider in an Insider World.
By : Olga Khazan
Date : April 24, 2020
Source : The Atlantic (https://www.theatlantic.com/health/archive/2020/04/could-there-be-another-coronavirus-quarantine/610630/)
Open science takes on the coronavirus pandemic
Data sharing, open-source designs for medical equipment, and hobbyists are all being harnessed to combat COVID-19.
When reports emerged in late 2019 of an outbreak of a new coronavirus centred in Wuhan, China, researchers at the virological-analysis website Nextstrain were ready. The open-source project tracks the spread of viruses through genetic variations in the sequences that scientists find. After five years of development and operation, Nextstrain had team members on three continents who could continuously refresh the analysis, 24 hours a day.
What they didn’t know was whether researchers would share their data. “You just never know what level of detail is going to be allowed to come out,” says Emma Hodcroft, a Nextstrain developer and molecular epidemiologist at the University of Basel in Switzerland.
But since 11 January, when a team led by Zhang Yong-Zhen at the Shanghai Public Health Clinical Center, China, shared the first genome sequence of the SARS-CoV-2 virus, the volume of data has skyrocketed. By the end of March, Nextstrain was receiving anywhere from 50 to 200 sequences a day from laboratories around the world, and was running its analysis of virus evolution every few hours. “The volume that we’re getting right now, this is totally unprecedented,” says Hodcroft.
Nextstrain is just one example of how an open ethos has driven the scientific response to the COVID-19 pandemic. Academics, online data repositories and home hobbyists with 3D printers are adopting new practices of rapid data sharing and collaboration that are appropriate to the urgency of the crisis. Many hope it will change the way science is done even after the pandemic subsides.
Do it yourself
Perhaps nowhere is that open ethos clearer than in the way do-it-yourself (DIY) and ‘maker’ communities have stepped up. As soon as it became clear that health systems around the world were at risk of running out of crucial equipment to treat people with COVID-19 and protect medical workers, DIY-ers set about trying to close the gap.
Facebook groups such as Open Source COVID19 Medical Supplies, which has more than 70,000 members, have become dispatch centres, through which hospital workers seek volunteers to print or make supplies, and volunteers trade tips on what materials to use and where to source them, and on sterilization procedures.
The coronavirus crisis plays to 3D printing’s strong points — rapid prototyping and the ability to produce parts on demand anywhere in the world. Prusa Research, a manufacturer of 3D printers in Prague, has designed a frame for a face shield that is meant to be worn outside a mask or respirator to protect against infectious droplets. The company says it has the capacity to produce 800 shields per day, and tens of thousands of the devices are already protecting health-care workers in the Czech Republic. But because the company made its designs open-source, they are also being made around the world in maker spaces and homes.
Formlabs, a 3D-printer manufacturer based in Somerville, Massachusetts, leads another project that has reached production: printing nasal swabs for COVID-19 test kits. Unlike common cotton swabs, nasal swabs must have a rod that is long and flexible enough to reach deep into the nose, to the upper throat. The swabs were designed by doctors at the University of South Florida in Tampa and the Northwell Health hospital system in New York, using printers purchased from the company to produce test versions. “They are prototyping it themselves, which is crazy and really awesome,” says Formlabs’s chief product officer, Dávid Lakatos. And whereas conventional swabs feature a bushy tip coating of nylon flock, the doctors devised a tip with an intricately textured pattern that is 3D-printed.
But unlike face shields, these parts are beyond the capabilities of most printers used by hobbyists. “If someone tried to print the swabs on a hobbyist printer, they can really do harm” in a clinical setting, says Lakatos.
Under US regulations, commercial manufacturing of nasal swabs must take place in a facility that has been registered with the US Food and Drug Administration (FDA). Formlabs has its own registered lab in Millbury, Ohio, with 250 printers (each costing about US$3,500) that can print 100,000 swabs a day.
The right tool
Other 3D-printed and DIY projects seek to provide everything from protective face masks for medical workers to door handles that can be opened using an elbow — helping health-care staff to avoid contaminating their hands — and ventilators for people who are critically ill. Among the furthest along in development are the OpenLung ventilator — a collaboration between groups based in Toronto, Canada, and Dublin — and the MIT Emergency Ventilator developed at the Massachusetts Institute of Technology in Cambridge. But manufacturing of such devices is still subject to regulatory approval. The MIT team told Nature that “approval would be sought by a manufacturer that ultimately adapts and makes a device inspired by the open-source reference material”. On 17 April, the first such device, called Spiro Wave, received Emergency Use Authorization from the FDA, making it available for use during the crisis; New York City has already ordered 3,000 units.
In the United Kingdom, a collaboration between University College London (UCL), the UCL Hospital and the Mercedes Formula One racing team has reverse-engineered and optimized a ‘continuous positive airway pressure’ device. The design has been approved by UK authorities for use during the COVID-19 pandemic and made available at no cost to manufacturers and researchers. The National Health Service has ordered up to 10,000 units. And in Nigeria, Yunusa Mohammed Garba, a researcher at Gombe State University, has built a positive-pressure ventilator from hobbyist and second-hand components, for use in the northeastern Gombe state, a resource-constrained part of the country. Nigeria has a population of about 200 million, yet it might have fewer than 500 ventilators. Garba’s design is currently being optimized and tested for use at the Federal Teaching Hospital Gombe, which plans to obtain two devices. “At the moment [the ventilator] can only be used in the ambulance,” Garba says. “We are currently using funding from the government to build an upgraded version of the ventilator that can be fully utilized in the hospitals.”
Still, even proponents of 3D printing find some of the projects potentially dangerous. “It’s both inspiring and extremely scary,” says Lakatos. Formlabs, for instance, investigated face-mask designs and produced numerous prototypes before recommending against 3D printing them. “The [3D-printed] face masks that I’m seeing, those designs are absolutely not sealing anything,” says Lakatos. “And I think they may be even giving a false kind of confidence to people.”
Following discussions with clinicians, Formlabs has instead been recommending a DIY respirator design produced by Boston Children’s Hospital in Massachusetts that repurposes off-the-shelf parts, including ventilator filters and a face mask used for administering anaesthetic gas. “It seems to be a much better solution than trying to do it with 3D printing,” says Lakatos.
One of the most widespread open-source face-shield designs eschews 3D printing entirely. The project began in March with the University of Wisconsin Makerspace in Madison, which worked with Midwest Prototyping, a 3D-printing company in nearby Blue Mounds, to produce them. But after bringing in Jesse Darley at the Madison office of Delve, an engineering design firm, the group decided to change tack. Instead of 3D printing, the frames and straps of the resulting ‘Badger Shields’ (named after the university’s mascot) are made from elastic and foam that can be purchased off-the-shelf in bulk form, and cut down either by machine or by hand. Darley says such components can be made in 20 seconds, compared with several hours through 3D printing.
The Madison group has already received orders for five million shields. To meet that demand, manufacturers have stepped in to help, including Ford Motor Company, which Darley says has tweaked the design for mass production and can make around one million shields per week.
Where credit’s due
The open ethos is influencing other aspects of the pandemic response, too. More than 2,000 articles on COVID-19 have been posted in the preprint archives bioRxiv and medRxiv, according to biomed-sanity.com, a site that aggregates preprints related to the pandemic. Numerous COVID-19 data sets are available on the code-sharing site GitHub, including the data underlying Johns Hopkins University’s widely used COVID-19 case-tracking dashboard. So, too, are reviews of the COVID-19 literature by researchers at the Icahn School of Medicine at Mount Sinai in New York City, and separately by a collaborative project led by computational biologists Halie Rando and Casey Greene at the University of Pennsylvania in Philadelphia.
Yet it wasn’t a given that researchers would embrace openness early in the outbreak: data that are made public can be difficult to publish through conventional channels later. And multiple news reports have suggested that health workers and researchers in China were initially subjected to government limits on what information they could release. But when Chinese researchers uploaded the first genome sequence of the SARS-CoV-2 virus to the online repositories virological.org and GenBank, they opened the floodgates for more sequences from China and from the rest of the world, Hodcroft says. “I am very grateful for the scientists who took this risk, because I think this set the precedent for the rest of the epidemic.” Given that the outbreak was initially confined to China, had those researchers not done so, “we might have completely different pictures that might be incorrect” she says.
Hodcroft hopes that these collaborative practices will carry over to research on other viruses and seasonal outbreaks. Not all labs have the equipment and personnel to sequence a viral genome, and even for those that do, the work requires time and money. But if more take that step — even if only every couple of weeks — she says it should be possible to track outbreaks in greater detail, using mutations as markers to better understand their geographical spread.
The pandemic could also bring lasting changes in how medical equipment is developed, produced and distributed. Lakatos would like to see hospitals have their own 3D printers as an emergency back-up to produce crucial equipment such as nasal swabs. And publicly available designs for parts such as face shields could make it easier to overcome breakdowns in international supply chains, allowing for more flexible, distributed manufacturing, says Darley.
Soon after releasing the Badger Shield plans, Darley was contacted by a company in Bonner, Montana, he had worked with that makes cycle rickshaws. The firm, called Coaster Cycles, had laid off or drastically cut hours for nearly all its workers because of the pandemic, but after seeing the open-source plans, it won a contract to supply shields to health systems spanning six US states — and hired back its workforce to produce them. Chief executive Ben Morris says the company eventually hopes to sell one million face shields. “That’s the power of open source,” says Darley. “It allows a family to make a few [units], or a manufacturer to make thousands, or hundreds of thousands.”
By : Mark Zastrow
Date : April 24, 2020
Source : Nature (https://www.nature.com/articles/d41586-020-01246-3)
Additional reporting by Abdullahi Tsanni in Abuja, Nigeria
doi: 10.1038/d41586-020-01246-3
How pandemics shape society
Johns Hopkins sociologist and historian Alexandre White discusses how past pandemics, such as the 1918 Spanish flu outbreak, have reverberated long after the disease stops spreading
From the bubonic plague of the 14th century to the Spanish flu outbreak in 1918, the repercussions and effects of pandemics have changed how societies function. Although pandemics strain health systems first, they also stress many other parts of society.
The Hub reached out to Alexandre White, an assistant professor of sociology and history of medicine at Johns Hopkins University, to learn more about the societal repercussions and consequences of past pandemics. This conversation has been edited for length and clarity.
How do international responses to the COVID-19 pandemic compare with those of previous pandemics?
That's a complicated question on a couple of levels. COVID-19, in a lot of ways, is a particularly effective disease at destabilizing health systems, as well as global economic processes. The fact that it can transmit asymptomatically and produce fairly mild symptoms in many of the cases means that its capacity to spread is quite high and it is putting a real strain on health systems around the world.
Since 1851, the threat of epidemic spread from particular diseases has been a critical concern for nations and the international community. The International Sanitary Conferences, which began in 1851, aimed to prevent the spread of infectious disease without disrupting trade and traffic. From the late 19th century through World War II, the ISC [oversaw the international response to] the spread of three diseases—plague, cholera, and yellow fever—until those responsibilities were transferred to what we now know as the World Health Organization.
The response by the WHO to COVID-19 was organized quite quickly. Since 2005, WHO regulations have established protocols and criteria for national health system readiness and also for what constitutes a "public health emergency of international concern," or PHEIC. WHO declared a PHEIC for COVID-19 at the end of January, which highlighted the severity of the threat. This was intended to aggressively mobilize international responses.
What we've actually seen in response to WHO's PHEIC declaration, particularly in the U.S. and the EU, has been a limited capacity for testing potential cases, which means that aspects of our treatment capacity are weakened.
The COVID-19 pandemic is frequently compared to the 1918 Spanish flu pandemic and the 2009 H1N1 outbreak. Are these fair comparisons?
I think that, biologically, comparing COVID-19 to previous flu outbreaks is useful because the process of epidemic spread can be similar. Like COVID-19, flus are often spread through droplets. The differences arise in the populations that are most at risk. We're still learning about the profile for those most at risk for COVID-19. Also, we have more effective diagnostic tools and biomedical responses now than we did in 1918, as well as increased capacity and knowledge in the medical sector. That puts us in a better position to confront this pandemic. However, in the absence of the pharmacological intervention, the practices of social distancing and quarantine initiatives might look similar to those of 1918.
An epidemic that's largely been overlooked in comparison to this one is the most recent West African Ebola virus disease epidemic, as well as the recent Ebola epidemic in Democratic Republic of Congo. In these epidemics, aggressive, long-term social distancing measures were put in place in countries like Guinea, Liberia, and Sierra Leone. Although Ebola is biologically different in its method of contagion, we might still be able to look at the effective social distancing strategies carried out in West Africa for solutions to this current pandemic.
I hope we can recognize that social distancing measures are taken out of an abundance of care for one another, and we should be vigilant about how these practices protect the ones we love and the health workers confronting this disease.
There has been a lot of postulating on how public health measures, like social distancing, might change the nature of society. Historically, what are the lingering effects of global pandemics on societies?
In Cape Town in 1901, a plague epidemic produced a very aggressive racial segregated quarantine that, in many ways, became the precursor and blueprint for future segregated towns and communities in apartheid South Africa. It's a stark example of how racism and bigotry can drive very aggressive and oppressive responses against those most marginalized in a society.
Epidemics are crises. During crises, a lot of commonly held beliefs are questioned, and the status quo can be thrown into question, too. It's my hope that we can see how public health and socioeconomic disparities are widening as a result of the COVID-19 pandemic. Ideally, this will lead us to create better systems in the future.
Have there been any indications that the COVID-19 pandemic is exacerbating these inequalities?
Unfortunately, yes. The dangerous framing of this particular pandemic as a "Chinese virus" or the "Wuhan virus" leads to a great deal of stigma for anyone from China or of Asian descent. It leads to violence, harassment, hatred, and bigotry, as we've already seen. The ways in which this pandemic has exacerbated these particular practices of bigoted and racist ideology is not surprising during an epidemic, but it's a serious threat to effective health responses.
We've seen time and time again, in responses to HIV/AIDS in the 1980s or in responses internationally to bubonic plague from the early 1900s, that stigma and bigotry—especially when diseases become associated with certain people and communities—have the effect of creating a potentially vindictive public health response. We don't want to steer people who are sick away from the health care that they need because they're afraid they'll be persecuted or stigmatized for their illness.
The second aspect I'd want to touch on is how epidemics highlight inequality. We're starting to see it now in the high rates of unemployment that are stretching the capacities of our existing social welfare network in the United States. There have been very few national initiatives thus far for people who have been laid off from service work like employees at restaurants, in hospitality, and in recreation.
We are also seeing now how racial inequalities and existing health disparities are putting certain people at greater risk of severe symptoms and complications. These are the products of social inequality as much as epidemic dynamics. This needs to be addressed soon, and is emblematic of the declining social welfare network in the United States.
Date : April 9, 2020
By : Hub staff report
Source : https://hub.jhu.edu/2020/04/09/alexandre-white-how-pandemics-shape-society/
Coronavirus is spreading panic. Here’s the science behind why.
From prehistoric predator encounters to frantic toilet paper runs, our anxious brains can short-circuit when faced with the scary unknown.
Since the coronavirus began spreading across the world, we’ve learned a lot about the lengths to which people will go for a roll of toilet paper, a tube of hand sanitizer or a face mask. As the number of confirmed coronavirus cases increases and states and countries lock down large gatherings or shops to promote social distancing, these uncertainties are driving the so-called “panic-buying” that’s emptying store shelves quicker than they can be restocked.
Panic-buying supplies is one way humans have coped with uncertainty over epidemics since at least 1918 during the Spanish flu—when people in Baltimore raided drug stores for anything that would prevent the flu or relieve its symptoms—all the way up to the 2003 SARS outbreak.
“When you’re seeing extreme responses. It’s because people feel like their survival is threatened and they need to do something to feel like they’re in control,” explains Karestan Koenen, professor of psychiatric epidemiology at the Harvard T.H. Chan School of Public Health.
But what exactly causes us to panic—and how can we keep our cool in a high-stress time like a pandemic? It depends on how different areas of the brain play along with each other.
The evolution of fear and panic
Human survival has depended on both fear and anxiety, requiring us to react immediately when we encountered a threat (think: the lion around the corner) as well as being able to mull over perceived threats (where are the lions tonight?)
Panic starts when a negotiation of sorts in the brain goes awry. Koenen explains that the amygdala, the emotional center of the brain, wants us to get out of harm’s way immediately—and it doesn’t care how we avoid the lion.
But the frontal cortex, which handles your behavioral responses, insists that we think the lion situation through first. When might we run into a lion again, and what to do about it?
Sometimes anxiety can get in the way. Rather than talking directly to the parts of our brains that are good at planning and making decisions, the frontal cortex gets confused by all the cross-talk between other parts of the brain that are determined to play out all the possible scenarios for how we might become a lion’s dinner.
Panic happens when the whole thing short-circuits.
While our frontal cortex wants to think about where the lions may be tomorrow night, our amygdalas are in overdrive.
“Panic happens when that more rational part of your brain [the frontal cortex] gets overrun by emotion,” Koenen says. Your fear is so acute that the amygdala takes over and adrenaline kicks in.
In certain scenarios, panic can be life-saving. When we’re in immediate danger of being mauled by a lion or run over by a car, the most rational response may be flight, fight, or freeze. We don’t want our brains to spend too much time debating that.
But listening just to the amygdala can come with serious drawbacks. In his 1954 work, “The Nature and Conditions of Panic,” Enrico Quarantelli, a sociologist who conducted ground-breaking research on how humans behave during disasters, told the story of a woman who heard an explosion and fled her house, thinking a bomb had hit it. It was only when she realized the explosion had occurred across the street that she remembered she had left her baby behind.
“Panic, rather than being antisocial, is a nonsocial behavior,” Quarantelli wrote. “This disintegration of social norms… sometimes results in the shattering of the strongest primary group ties.”
Panic doesn’t help much with long-term threats either. That’s when it’s essential for the frontal cortex to remain in control, alerting you to the possibility of a threat while also taking the time to assess the risk and make a plan to act.
How uncertainty can drive panic
But if we’re deluged with information and messaging during this pandemic, why are some people hoarding toilet paper and hand sanitizer during this pandemic while others are dismissing the risks and packing into bars?
Humans are notoriously bad at assessing risk in the face of uncertainty—and we’re often bad at it in different ways that cause us to overestimate or underestimate our personal risks.
Sonia Bishop, an associate professor of psychology at the University of California Berkeley who researches how anxiety affects decision-making, says that’s particularly true now during the coronavirus pandemic. Inconsistent messaging from governments, the media, and public health authorities—such as all the varied recommendations on social distancing—fuels anxiety.
“We’re not used to living in situations where we have rapidly changing probabilities,” Bishop says.
Panic and our psychological biases
Ideally, Bishop says, we should be taking an approach called model-free learning to assess our risk in the face of uncertainty. This approach is essentially trial and error: we rely on our personal experiences and gradually update our estimates of how likely something is to happen, how bad it would be if it does happen, and how much effort we need to put in to prevent it.
When we don’t have a model for how to handle a threat, Bishop says, many people turn to model-based learning, a framework in which we either try to recall examples from the past or simulate future possibilities.
And that’s where “availability bias” creeps in. When we’ve heard or read about something a lot—for instance, a plane crash covered extensively in the news—it becomes so easy to imagine oneself in a plane that’s crashing that one may overestimate the risk of flying. “It’s that ease of simulating that scenario that then overwhelms our judgements of the probability,” Bishop says.
Similarly, some people have biases toward optimism or pessimism. While pessimists can’t stop anxiously imagining all the potential doomsday scenarios, optimists tend to believe that nothing bad is going to happen. Even if they fall into one of the vulnerable groups, they find a way to reconcile that with their worldview by assuring themselves that they are too healthy to die from the coronavirus. “It gives you back some [sense of] control,” Bishop says.
Is there ever a good time to panic?
While there certainly are people behaving on either side of these extremes, most people are experiencing something else: acute anxiety.
Some amount of anxiety can be good in the face of disaster. Fear can be a motivator, raising our alertness and energy levels. It reminds us to wash our hands, pay attention to the news—and, yes, even stock up on essentials at grocery stores.
Jennifer Horney, founding director of epidemiology at the University of Delaware and a public health preparedness expert, points out that a little more panic could be particularly helpful in a place like the U.S., whose population historically has not as good as other countries’ when it comes to following public health interventions such as isolation and quarantine.
“In that sense maybe a little more panic might be productive in terms of understanding that our behavior does impact others,” she says.
On the other hand, anxiety is a terrible thing to suffer from over the long term. For one thing, as we become more anxious, it’s also harder for our brains to keep from spiraling into panic mode. Studies have indicated that chronic stress can actually shrink the parts of our brains that help us reason, which can further fuel panic.
Bishop points out that our bodies really aren’t made to live with acute stress and anxiety for weeks and months. Though they may give us a short term energy burst, it ultimately leaves us exhausted and depressed. This can ultimately have serious implications for society’s response if people get so burned out on social distancing that they start going out again before the pandemic has hit its peak.
Panic and pandemic interventions
Horney, who trained rapid response teams during the 2009 H1N1 (“Swine Flu”) pandemic, says reducing uncertainty is key to ensuring that our interventions do work.
Coronavirus is not a complete unknown, she notes. Public health officials also know a lot about coronaviruses from dealing with SARS and MERS.
“A lot of the things that are happening are the typical public health measures that we take to control outbreaks; it’s just happening on a much larger scale,” Horney says.
“We quarantine cruise ships all the time because of outbreaks, but it’s usually norovirus or seasonal influenza.”
Date : March 17, 2020
By : Amy Mckeever
Source : https://www.nationalgeographic.com/history/reference/modern-history/why-we-evolved-to-feel-panic-anxiety/
Social distancing prevents infections, but it can have unintended consequences
In response to the coronavirus pandemic, public health officials are asking us to do something that does not come naturally to our very social species: Stay away from each other. Such social distancing—avoiding large gatherings and close contact with others—is crucial for slowing the spread of the virus and preventing our health care system from getting overwhelmed. But it won’t be easy.
“The coronavirus spreading around the world is calling on us to suppress our profoundly human and evolutionarily hard-wired impulses for connection: seeing our friends, getting together in groups, or touching each other,” says Nicholas Christakis, a social scientist and physician at Yale University.
And social distancing also tests the human capacity for cooperation, he adds. “Pandemics are an especially demanding test … because we are not just trying to protect people we know, but also people we do not know or even, possibly, care about.”
The effects of short-term social distancing haven’t been well studied, but several researchers—most of them scrambling to deal with disruptions to their own lives because of the coronavirus—recently took time to share some thoughts with ScienceInsider on the potential social and psychological impacts, and how to mitigate them. Here’s what they said:
What’s known about the effects of social interaction on mental and physical health?
Over long periods of time, social isolation can increase the risk of a variety of health problems, including heart disease, depression, dementia, and even death. A 2015 meta-analysis of the scientific literature by Julianne Holt-Lunstad, a research psychologist at Brigham Young University, and colleagues determined that chronic social isolation increases the risk of mortality by 29%.
That may be because social contacts can buffer the negative effects of stress. Lab studies by Holt-Lunstad and others have found that having a friend present can reduce a person’s cardiovascular response to a stressful task. There’s even a correlation between perceived social connectedness and stress responses. “Just knowing that you have someone you can count on if needed is enough to dampen some of those responses even if [that person is] not physically present,” Holt-Lunstad says.
What effects, if any, might be caused by social distancing in response to the coronavirus is an open question. “I have a couple competing hypotheses,” Holt-Lunstad says. “On the one hand, I am concerned that this will not only exacerbate things for those who are already isolated and lonely, but also might be a triggering point for others to now get into habits of connecting less.”
A more optimistic possibility, she says, is that heightened awareness of these issues will prompt people to stay connected and take positive action. “We’d love to be collecting data on that,” she says.
Are certain people or populations more likely to be affected?
People of all ages are susceptible to the ill effects of social isolation and loneliness, Holt-Lunstad says. But a recent report from the National Academy of Sciences (of which she was a co-author) highlights some reasons older people may be more susceptible, including the loss of family or friends, chronic illness, and sensory impairments like hearing loss that can make it harder to interact.
There’s enormous individual variation in people’s ability to handle social isolation and stress, adds Chris Segrin, a behavioral scientist at the University of Arizona. It’s important to remember that not everyone is going into this with the same level of mental health, he says. “Someone who is already having problems with, say, social anxiety, depression, loneliness, substance abuse, or other health problems is going to be particularly vulnerable.”
Overall, though, people are remarkably resilient. And many have endured far worse situations. Segrin points to case studies of U.S. prisoners during the Vietnam War who were confined in tiny cells called “tiger cages,” sometimes in water up to their chin. One trait that predicted their long-term psychological health was optimism: Prisoners who believed that, no matter how bad things were, they would survive and the war would eventually be won had better mental health later on in life.
Can technology help compensate for some of the downsides of social distancing?
Texting, email, and apps like Skype and FaceTime can definitely help people stay in touch. “We are fortunate to live in an era where technology will allow us to see and hear our friends and family, even from a distance,” Christakis says.
Even so, those modes of communication don’t entirely replace face-to-face interactions, Segrin says. “When we interact with other people, a lot of the meaning conveyed between two people is actually not conveyed in the actual words, but in nonverbal behavior,” he says. A lot of those subtleties of body language, facial expressions, and gestures can get lost with electronic media. “They’re not as good as face to face interactions, but they’re infinitely better than no interaction,” Segrin says.
What will we miss by not being able to go to things like concerts and sporting events?
One hundred years ago, French sociologist Émile Durkheim used the phrase “collective effervescence” to describe the shared emotional excitement people experience during religious ceremonies. The same concept applies to sporting events where spectators simultaneously experience the rise and fall of emotions during the course of a game, says Mario Small, a sociologist at Harvard University. “It dramatically magnifies the sensation for you while also reinforcing the idea that you’re something larger than yourself,” Small says.
Such events help build cohesiveness, he says, and although no one expects society to fall apart just because NBA and other sports leagues have suspended their seasons, for many sports fans (and music fans and festival goers) the growing list of canceled events represents another coping mechanism they’ll have to temporarily get by without.
What else can we do?
“Any one of us can pick up a phone and call to see how people are doing and what they might need,” Holt-Lunstad says. She notes that research on altruism has found that giving support can be even more beneficial than receiving it. “Not only will helping others potentially help them, but it can help us to still feel connected as well.”
There’s also the inspiration of people under lockdown in Italy singing and playing music through open windows to keep spirits up. “That’s the kind of thing we need!” says Robin Dunbar, an evolutionary psychologist at the University of Oxford. “But maybe only the Italians would have the flair to do that without being embarrassed,” he adds. The rest of us, it seems, will have plenty of time to work up the nerve.
Date : March 16, 2020
By : Greg Miller
Source : https://www.sciencemag.org/news/2020/03/we-are-social-species-how-will-social-distancing-affect-us#
Using sociology to make sense of the coronavirus pandemic
'We must begin with the kind of mind that links our personal circumstances with the public experience'
It is apparent that the coronavirus pandemic is trouble for every individual. But there is a caveat to this.
Sociologist C. Wright Mills proposes that our personal troubles should be understood in light of public issues. More often than not, we do not link our personal troubles with the issues of society as a whole. We might think that our personal troubles – in this case, safety from the virus – can be solved through our individual coping mechanisms alone. But one thing is certain: the coronavirus is a public issue.
But the mere recognition of the issue as a public concern is just the beginning. Making sense of this phenomenon is another task. German sociologist Ulrich Beck’s notion of “risk society” will be helpful here.
He describes the contemporary world as one where people, governments, and corporations are increasingly mindful of the experience of risk in different aspect of our lives, including health. He says that in the event of any world catastrophe, the impact would be damaging and difficult to contain. We see this social reality in the increasing number of deaths worldwide and in the different measures, rules, and regulations imposed by different states.
How, then, should we deal with the phenomenon of the coronavirus as a public issue and a global risk?
Date : March 26, 2020
By : Prince Kennex R. Aldama
Source : https://www.rappler.com/views/imho/255954-opinion-using-sociology-make-sense-coronavirus-pandemic
Sociologist explains how coronavirus might change the world around us
In his role as a medical sociologist, Richard M. Carpiano studies population health issues, analyzing how a variety of social factors influence both the physical and mental health of people around the world.
Carpiano is a professor of public policy and sociology at the University of California, Riverside. Most recently, his research has focused on vaccine hesitancy, or the reasons underlying whether parents might choose not to vaccinate their children or to delay vaccine coverage.
A pandemic like COVID-19 is especially interesting to sociologists because "it forces conversations by radically rearranging our social routines," Carpiano said. Below, he shares some insights about how the coronavirus could have far-reaching impacts on our social structures and routines.
As a sociologist, can you give us a bird's-eye view of how you approach a pandemic like COVID-19? What do you look at first?
For me, an event like this is especially notable because of its ability to reveal limitations in social policy. As a society, we can plan for so many human elements, but then here's a virus that comes along and shows all the weak links we have when it comes to things like family leave policy, unemployment policy, and public health policy.
What we often don't discuss when we talk about health care in the U.S. is our public health system. This situation is really bringing forward how important having a well-funded, well-organized public health system is in this country at the county, state, and national levels, and how important it is to have coordination between agencies. It's a sector that's been underinvested in for a long time, especially at the federal level, but as we're seeing, you really do get what you pay for.
In your research, you study how social conditions—and social inequities—influence health outcomes. How are you applying that lens to looking at the coronavirus?
Well, a pandemic like this doesn't hit everyone equally. Of course, with COVID-19 we see differences in risk based on age, and we can already see certain groups being more marginalized when it comes to being able to access resources such as testing and medical care. But in particular, this pandemic has highlighted the vulnerabilities of people in different types of occupations, many of whom belong to traditionally lower income brackets. It's revealed how closely our benefits are tied to our work, what happens when that work goes away, and ultimately how many Americans are in precarious work situations.
What about health impacts we might see as a result of people being isolated and having to dramatically change their usual routines?
There's been talk that we might see a coronavirus birth cohort as people are spending more time quarantined at home—it's certainly a time for intimacy, but a time for more conflict, too, as people are living on top of one another for long stretches. But we also might see a number of collateral health impacts from this pandemic, such as people being more sedentary, eating more out of boredom, and generally being less active. We might see alcohol consumption go up and substance abuse become more prevalent. I would imagine most people right now have less access to their doctors or are becoming less likely than usual to have their medications refilled. All of these things could lead to additional health consequences down the line.
Do you see any unexpected silver linings that could result from this situation?
I've been trying very hard, as a coping mechanism, to think of some positive things that could come out of this, and one thing I think might be a silver lining is that this event has really highlighted the importance of state government. People have a lot of criticisms about how the federal government has been handling this situation, and many of those are legitimate, but we're also seeing state officials really rise to the challenge and demonstrate leadership at a time when trust in government isn't exactly the highest. It's been an opportunity for a new wave of political leaders to step forward—people showing that it's not just about politics or partisanship, but really about being a public servant.
The reality is there are very few people who are anti-government in times of crisis. People look to government for direction on what to do. As a result of this, I think we might see more trust in state government, in particular.
Are there any historical events you view as similarly disruptive to society or are looking to in comparison?
It might be because I was in New York when 9/11 happened, but that's what my mind goes to. That was another situation where the U.S. was taken off guard and had its governmental limitations exposed very suddenly—major limitations in operation, planning, and problem-solving. But in the wake of 9/11, we saw a real public push to figure out how this happened and how we could prevent it from happening ever again. We saw the formation of the 9/11 Commission and a lot of other significant changes made in the realms of foreign policy and national security. I'm hoping a similar trend might take hold after this, but in relation to public health and promoting new conversations about what we can do to prevent something similar from happening again by strengthening our public health system.
You also study vaccine hesitancy, or the reasoning behind why some parents might not choose to have their children vaccinated. Do you think this situation could have any bearing on changing public perception of vaccines to help skeptics view them more favorably?
Vaccines are not a bread-and-butter issue for the average American; most people in this country support them. If anything, I think, this situation could help raise support for elected officials to enact stricter measures to ensure the population's vaccination coverage is as high as it can be. But when we look at the very small minority of vocal, dyed-in-the-wool groups who are anti-vaccines and actively lobby against them, I'm unfortunately not very optimistic that this event will change their minds much. We're already seeing a lot of conspiracy theorizing surrounding this situation from them, and they tend to equate vaccine requirements with "government overreach" no matter what. But one thing I think we might see is their usual tactics not working as well when it comes to getting the ears of elected officials.
Date : April 2, 2020
By : Tess Eyrich, University of California – Riverside
Source : https://phys.org/news/2020-04-sociologist-coronavirus-world.html
Poor city dwellers run greatest coronavirus risk
BARCELONA, April 9 (Thomson Reuters Foundation) - In working-class Roquetes, life looks good: the Mediterranean glitters on the horizon and sun dapples the green hills behind. But in the coronavirus crisis, this modest Barcelona neighbourhood faces grave risk.
Residents are seven times more likely to get COVID-19 than people in wealthier districts of Spain’s second city, according to an interactive map published by regional authorities.
The rate of infection in Roquetes, among the Nou Barris - or ‘New Districts’ - of Barcelona, is 533 per 100,000 inhabitants, according to the map, which tracked COVID-19 across Catalonia.
About 6 km away, in the upmarket area of Sant Gervasi, the rate of infection is just 77.
Spain is among the worst hit nations in the global crisis, with some 150,000 cases and its big cities suffering most.
Nor is the Roquetes district an inner-city exception.
In El Prat de Llobregat and Sant Quirze del Vallès – working-class satellite towns just outside Barcelona – the rate of infection is even higher, at 604 and 701 per 100,000 inhabitants respectively.
These stark urban inequalities are mirrored in busy cities across the world, showing just what money can buy.
Health experts hope the Barcelona map, along with a slew of others tracking the spread of the new coronavirus, helps the world to recalibrate in COVID-19’s aftermath and better protect those city dwellers most at risk from disease.
Socio-economic status is the biggest factor in determining whether someone in Barcelona will contract the virus or not, said Mark Nieuwenhuijsen, a professor of environmental epidemiology at the Barcelona Institute for Global Health.
“In places like Nou Barris, where you see the highest risk, there is less education around, people are probably less aware of these kinds of things but also need to travel more for jobs,” he told the Thomson Reuters Foundation by phone.
“Poorer people often do jobs that mean they have to get around - like working in shops or running public transport systems,” he said, while the wealthy can often work from home and so are less likely to come into contact with the virus.
POVERTY
Urban health experts say busy western hubs share many similarities with Asian cities, whose crowded neighbourhoods and slums are particularly vulnerable to disease outbreaks.
“Refugee and minority populations live in poor quality, densely occupied accommodation with insecure working conditions,” said Carolyn Stephens, a professor of global health at University College London.
Aside from the ease of contagion in dense neighbourhoods, a poor standard of living carries wider risks, said Herbert Gans, a sociology professor at Columbia University.
“Poverty has an almost endless number of bad effects, beginning with poor health, a weak immunity system and low resistance, insufficient medical care, unhealthy housing, and so on,” Gans told the Thomson Reuters Foundation.
In New York, for instance, the rate of people who have tested positive in Queens and the Bronx far outstrips that of people living in the wealthier borough of Manhattan, according to data released by New York City’s Health Department.
“Urban density may play a role, as with this you tend to have more human contact, but I don’t think it’s the determining factor,” Nieuwenhuijsen concurred.
Date : April 9, 2020
By : Sophie Davies, Thomson Reuters Foundation
Source : https://www.reuters.com/article/health-coronavirus-innercity/feature-poor-city-dwellers-run-greatest-coronavirus-risk-idUSL8N2BV2HD


